Section A:
Concussion Recognition, Initial Medical Assessment, Return to School and Activity
Introduction
The majority of children and adolescents with an acute concussion will make a complete recovery within 1-4 weeks. Those with prolonged symptoms (symptoms that last more than 4 weeks following the acute injury) can benefit from a referral to interdisciplinary teams and experienced healthcare professionals who are optimally trained to evaluate and treat the heterogeneous causes of these symptoms. For those at risk of a prolonged recovery, specialized interdisciplinary concussion care is ideally initiated within the first two weeks post-injury. When providing medical clearance to return to activities with a risk of future concussion, patients should be managed on an individualized basis. Interdisciplinary concussion teams may be recommended to manage recovery in situations in which patients have prolonged symptoms, complex medical histories, repeated concussions, or pre-injury conditions or diagnoses.
Medical and healthcare professionals should work together with patients, their families, and those involved in their lives (teachers, coaches, employers, friends, etc.) using a team and family-centred approach to best manage the needs of the patient after a concussion and promote positive health outcomes. Proper concussion recognition in children and adolescents requires all involved in a child’s life to be educated on the signs and symptoms of this condition and to collaborate to ensure that youth with suspected concussion are immediately removed from play or activity and directed to the most appropriate care. The following sections provide recommendations specific to concussion recognition, initial medical assessment, and management.
Guideline Tools:
- Tool 1.3: Manage Acute and Prolonged Symptoms Algorithm
- Tool 2.0: Living Guideline Return to Activity Sports and School Protocol
- Tool 2.1 Physical Examination
- Tool 2.2 PECARN Management Algorithm for Children after Head Trauma.
- Tool 2.3 CATCH2 Rule
- Tool 2.4: Algorithm for the Management of the Pediatric Patient ≥ 2 years with Minor Head Trauma
- Tool 2.5: “Four P’s” – Prioritize, Plan, Pace, and Position
- Tool 2.6: Post-Concussion Information Sheet
- Tool 2.7: Strategies to Promote Good Sleep and Alertness
Concussion Recognition and Directing to Care
Introduction:
Recommendations
LEVEL OF EVIDENCE  A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study)
A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study) B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations)
B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations) C = Consensus, usual practice, opinion or weaker-level evidence
C = Consensus, usual practice, opinion or weaker-level evidence
1.1a
School boards, sports organizations, and community centres should provide pre-season concussion education and conduct a review of all concussion policies in effect within the school or sport setting.
Level of Evidence: ![]()
1.1b
School boards, sports organizations, and community centres should ensure updated policies are in place to recognize and accommodate a child/adolescent who has sustained a concussion.
Level of Evidence: ![]()
1.2
Remove the child/adolescent from the activity immediately if a concussion is suspected to avoid further injury and have the child/adolescent assessed.
Do not leave the child alone and contact the parent/caregiver immediately. Do not let the child/adolescent return to sport (practice or game play) or other physical activities that day. “If in doubt, sit them out.”
A concussion should be suspected:
- In any child/adolescent who sustains a significant impact to the head, face, neck, or body and demonstrates/exhibits any of the visual signs of a suspected concussion or reports any symptoms of a suspected concussion as detailed in the Concussion Recognition Tool 6 (Tool 1.2).
Premature return to activities and sport can lead to another injury. Another blow to the head may complicate the injury further and result in a longer recovery time (i.e, higher risk of persisting symptoms). Severe brain swelling or cerebral edema after a concussion is very rare but potentially fatal.
Level of Evidence: ![]()
Online Tools to Consider
- Concussion Recognition Tool 6 (Tool 1.2)
- Living Guideline Patient Information Sheet (includes return to sport/activity and school protocols)
- Link: Parachute Concussion Guidelines for Parents & Caregivers (handout- Parachute Canada) (UPDATE IN PROGRESS)
- Link: Concussion Ed – Parachute Concussion Education (app- Parachute Canada)
- Link: PAR Concussion Recognition & Response: Concussion symptom recognition tool for coaches and parents (app)
- Link: CATT: Concussion Resources for School Professionals (handout)
- Link: CATT Concussion Resources for Coaches (handout)
1.3
Recommend an emergency medical assessment for a child/adolescent with any of the “red flag” symptoms.
If a child/adolescent demonstrates any of the ‘Red Flags’ symptoms indicated by the Concussion Recognition Tool 6, a more severe head or spine injury should be suspected and an emergency medical assessment is required. These red flag symptoms may appear immediately or within a few hours or days after injury. Delayed red flag symptoms require urgent medical assessment as they may indicate a more severe injury. Consider arranging an ambulance service as necessary to facilitate urgent medical assessment at the nearest hospital and execution of the Emergency Action Plan for your organization. When calling an ambulance, describe the specific red flags symptoms over the phone.
Red flag symptoms include:
- Severe or increasing headache
- Neck pain or tenderness
- Double vision or loss of vision
- Weakness or numbness/tingling in extremities
- Seizure or convulsions
- Loss of consciousness
- Increased confusion or deteriorating conscious state
- Repeated vomiting
- Increasingly restless, agitated or combative state
- Slurred speech
- Visible skill deformity
Level of Evidence: ![]()
Online Tools to Consider:
- Tool 1.2 Concussion Recognition Tool 6 (handout)
- Link: Concussion Ed – Parachute Concussion Education (app)
- Link : PAR Concussion Recognition & Response (app)
1.4
Concussion should be suspected and diagnosed as soon as possible to maintain health and improve outcomes. Concussion can be suspected in the community by healthcare professionals, parents, teachers, coaches, and peers. Those with a suspected concussion should be assessed by a physician or nurse practitioner to perform a thorough medical assessment to exclude more severe injuries, consider a full differential diagnosis, and confirm the diagnosis of concussion.
It is important to note that some patients may experience a delayed onset of concussion symptoms. Delayed concussion symptoms also require medical assessment to exclude more severe injuries.
- Tool 1.2: Concussion Recognition Tool 6
- Tool 1.3: Manage Acute and Prolonged Concussion Symptoms Algorithm
- Symptoms may appear immediately or within several hours after injury.
- A concussion is an evolving injury; symptoms may change over time.
- See Recommendation 1.3 above: Recommend emergency assessment for a child/adolescent with any of the “red flag” symptoms.
Level of Evidence: ![]()
Online Tools to Consider:
-
Sport Concussion Assessment Tool 6 (SCAT6 13+yrs and Child SCAT6 8-12yrs) – for experienced healthcare professionals to suspect a concussion:
Tools and Resources
Living Guideline Tools
- Tool 1.1: Pediatric Concussion: The Role of School Boards, Community Sports Organizations, and Centres
- Tool 1.2: Concussion Recognition Tool 6. To help identify concussion in children, adolescents, and adults (updated Sept 2023)
- Tool 1.3: Manage Acute and Prolonged Symptoms Algorithm
Links to Toolkits and Online Resources for School Concussion Policies:
- 2016 Berlin Consensus in Sport Group Statement
- Advice for gradually resuming activities after a concussion: Institut national d’excellence en sante et en services sociaux (INESSS- Québec) English / French
- An Educator’s Guide to Concussions in the Classroom, 2nd Edition: Nationwide Children’s Hospital, Columbus, OH
- A Roadmap for Implementing Concussion Management Policies and Protocols in Sport (CASEM)
- Canadian Guideline on Concussion in Sport Pre-Season Education Sheet (Parachute)
- Concussion Awareness Training Tool: CATT Online
- Concussion Ed – Parachute Concussion Education (App)
- HEADS UP Concussion and Helmet Safety App (CDC)
- Parachute: Canadian Guideline for Concussion in Sport (Update in proxgress)
- Parachute Concussion Series: After a Concussion Return to Sport strategy (Update in progress)
- Parachute Concussion Series: Concussion Guide for Teachers
- SCHOOLFirst Handbook: Enabling successful return to school for Canadian youth following a concussion (Holland Bloorview Kids Rehabilitation Hospital)
- Ontario Ministry of Education School Board Policies for Concussion
Concussion Recognition and Directing to Care Online Tools to Consider:
- CATT: Concussion Resources for School Professionals (handout)
- CATT Concussion Resources for Coaches (handout)
- Concussion Ed – Parachute Concussion Education (app)
- PAR Concussion Recognition & Response: Concussion symptom recognition tool for coaches and parents (app)
- Parachute Concussion Guidelines for Parents & Caregivers (handout)
- Sport Concussion Assessment Tool 6 (SCAT6 13+yrs and Child SCAT6 8-12yrs) (Updated Sept 2023)
- Sport Concussion Office Assessment Tool (SCOAT6 13+ yrs and Child SCOAT6 8-12 yrs) (Updated Sept 2023)
References
Updated Living Guideline Evidence Map (stratified by Domain)
Previous reference list:
Amit, Perlin, and Kroshus Emily. 2020. “Content Analysis of Concussion Education for Coaches of Youth and High School Sport.” Brain Injury 34 (7): 905–13. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medl&NEWS=N&AN=32362145.
Charek Daniel, R J Elbin, Sufrinko Alicia, Schatz Philip, D’Amico Nathan R, Collins Michael W, and Kontos Anthony P. 2020. “Preliminary Evidence of a Dose-Response for Continuing to Play on Recovery Time After Concussion.” The Journal of Head Trauma Rehabilitation 35 (2): 85–91. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medl&NEWS=N&AN=31033740.
Bara, Alsalaheen, Almeida Andrea, Eckner James, Freeman Jeremiah, Ichesco Ingrid, Popovich Michael, Streicher Nicholas, and Lorincz Matthew. 2021. “Do Male and Female Adolescents Report Symptoms Differently after Concussion?” Brain Injury 35 (6): 698–704. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medl&NEWS=N&AN=33689531.
Clark, Ricketta, Ansley Grimes Stanfill, Clark Ricketta, and Stanfill Ansley Grimes. 2019. “A Systematic Review of Barriers and Facilitators for Concussion Reporting Behavior among Student Athletes.” Journal of Trauma Nursing 26 (6): 297–311. https://doi.org/10.1097/JTN.0000000000000468.
Donnell, Zoe, Rosanne Hoffman, Kelly Sarmiento, and Cameron Hays. 2018. “Concussion Attitudes, Behaviors, and Education among Youth Ages 12–17: Results from the 2014 YouthStyles Survey.” Journal of Safety Research 64: 163–69. https://doi.org/10.1016/j.jsr.2017.12.001.
Fremont, Pierre, Kathryn Schneider, Anne Laroche, Carolyn Emery, and Keith Yeates. 2020. “Could a Massive Open Online Course Be Part of the Solution to Sport-Related Concussion? Participation and Impact among 8368 Registrants.” BMJ Open Sport and Exercise Medicine 6 (1): 1–7. https://doi.org/10.1136/bmjsem-2019-000700.
Howell, David R., Michael J. OʼBrien, Joana Fraser, and William P. Meehan. 2018. “Continuing Play, Symptom Severity, and Symptom Duration After Concussion in Youth Athletes.” Clinical Journal of Sport Medicine 0 (0): 1. https://doi.org/10.1097/jsm.0000000000000570.
Jill, Daugherty, DePadilla Lara, and Sarmiento Kelly. 2020. “Assessment of HEADS UP Online Training as an Educational Intervention for Sports Officials/Athletic Trainers.” Journal of Safety Research 74: 133–41. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem6&NEWS=N&AN=32951774.
Haarbauer-Krupa Juliet, Register-Mihalik Johna K, Nedimyer Aliza K, Chandran Avinash, Kay Melissa C, Gildner Paula, and Kerr Zachary Y. 2021. “Factors Associated with Concussion Symptom Knowledge and Attitudes towards Concussion Care-Seeking among Parents of Children Aged 5-10years.” Journal of Safety Research 78: 203–9. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem&NEWS=N&AN=34399916.
Kelly, Sarmiento, Daugherty Jill, and DePadilla Lara. 2019. “Youth and High School Sports Coaches’ Experience with and Attitudes about Concussion and Access to Athletic Trainers by Sport Type and Age of Athlete Coached.” Journal of Safety Research 69: 217–25. https://doi.org/10.1016/j.jsr.2019.01.005.
Kelly, Sarmiento, Donnell Zoe, Bell Elizabeth, Tennant Bethany, and Hoffman Rosanne. 2019. “A Qualitative Study of Barriers and Opportunities for Concussion Communication and Management among Parents of Youth Sports Athletes.” Journal of Concussion 3: 205970021986186–205970021986186. https://doi.org/10.1177/2059700219861863.
Weber Michelle, Welch Bacon, E Cailee, and McLeod Tamara Valovich. 2019. “School Nurses’ Management and Collaborative Practices for Student-Athletes Following Sport-Related Concussion.” The Journal of School Nursing : The Official Publication of the National Association of School Nurses 35 (5): 378–87.
Lara, DePadilla PhD, Miller PhD Gabrielle F, Everett Jones PhD, MPH, JD, and Sherry. 2020. “Characteristics of Schools with Youth Sports Concussion-Related Educational Policies and Practices.” Journal of School Health 90 (7): 520–26. https://doi.org/10.1111/josh.12900.
Lara, DePadilla PhD, Miller PhD Gabrielle F, Everett Jones PhD, MPH, JD, Sherry, Lara DePadilla PhD, Gabrielle F. Miller PhD, and Sherry Everett Jones PhD, MPH, JD. 2020. “Characteristics of Schools with Youth Sports Concussion-Related Educational Policies and Practices.” Journal of School Health 90 (7): 520–26. https://doi.org/10.1111/josh.12900.
Linder, Susan M., Jason Cruickshank, Nicole M. Zimmerman, Richard Figler, and Jay L. Alberts. 2019. “A Technology-Enabled Electronic Incident Report to Document and Facilitate Management of Sport Concussion: A Cohort Study of Youth and Young Adults.” Medicine 98 (14): e14948. https://doi.org/10.1097/MD.0000000000014948.
M, Black Amanda, Yeates Keith Owen, Babul Shelina, Nettel-Aguirre Alberto, and Emery Carolyn A. 2020. “Association between Concussion Education and Concussion Knowledge, Beliefs and Behaviours among Youth Ice Hockey Parents and Coaches: A Cross-Sectional Study.” BMJ Open 10 (8): e038166. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem&NEWS=N&AN=32830117.
Matveev, Roman, Lauren Sergio, Jessica Fraser-Thomas, and Alison K. Macpherson. 2018. “Trends in Concussions at Ontario Schools Prior to and Subsequent to the Introduction of a Concussion Policy – An Analysis of the Canadian Hospitals Injury Reporting and Prevention Program from 2009 to 2016.” BMC Public Health 18 (1): 1–10. https://doi.org/10.1186/s12889-018-6232-9.
McCart, Melissa, Ann E. Glang, Jody Slocumb, Jeff Gau, Laura Beck, and Doug Gomez. 2019. “A Quasi-Experimental Study Examining the Effects of Online Traumatic Brain Injury Professional Development on Educator Knowledge, Application, and Efficacy in a Practitioner Setting.” Disability and Rehabilitation 0 (0): 1–7. https://doi.org/10.1080/09638288.2019.1578423.
McGuine, Timothy A., Adam Y. Pfaller, Eric G. Post, Scott J. Hetzel, Alison Brooks, and Steven P. Broglio. 2018. “The Influence of Athletic Trainers on the Incidence and Management of Concussions in High School Athletes.” Journal of Athletic Training 53 (11): 1017–24. https://doi.org/10.4085/1062-6050-209-18.
Noelle, Yumul Joy, Crowe Louise, Catroppa Cathy, Anderson Vicki, and McKinlay Audrey. 2021. “Post-Concussive Signs and Symptoms in Preschool Children: A Systematic Review.” Neuropsychology Review. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medp&NEWS=N&AN=34390464.
Plourde, Vickie, Janice Y. Kung, Allison Gates, Shelly Jun, Brian L. Brooks, Meghan Sebastianski, Plourde Vickie, et al. 2020. “How Perceptions Impact Recovery from Concussion in Childhood and Adolescence: A Systematic Review.” Neuropsychology Review 30 (1): 142–63. https://doi.org/10.1007/s11065-020-09430-y.
Ricketta, Clark, and Stanfill Ansley Grimes. 2019. “A Systematic Review of Barriers and Facilitators for Concussion Reporting Behavior among Student Athletes.” Journal of Trauma Nursing 26 (6): 297–311. https://doi.org/10.1097/JTN.0000000000000468.
Robyn, Feiss, Lutz Molly, Reiche Elaine, Moody Justin, and Pangelinan Melissa. 2020. “A Systematic Review of the Effectiveness of Concussion Education Programs for Coaches and Parents of Youth Athletes.” International Journal of Environmental Research and Public Health 17 (8). https://doi.org/10.3390/ijerph17082665.
Robyn, Feiss, Lutz Molly, Reiche Elaine, Moody Justin, Pangelinan Melissa, Robyn Feiss, Molly Lutz, Elaine Reiche, Justin Moody, and Melissa Pangelinan. 2020. “A Systematic Review of the Effectiveness of Concussion Education Programs for Coaches and Parents of Youth Athletes.” International Journal of Environmental Research and Public Health 17 (8): 2665. https://doi.org/10.3390/ijerph17082665.
Ruikang, Liu, and Hicks Steven D. 2021. “Discrepancies in Child and Parent Reporting of Concussion Symptoms.” Brain Injury, 1–7. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medp&NEWS=N&AN=33646888.
Shendell, Derek G., Lauren Gonzalez, Tracy A. Listwan, Joseph Pancella, Mary Blackborow, and Joanna Boyd. 2019. “Developing and Piloting a School-Based Online Adolescent Student-Athlete Concussion Surveillance System.” Journal of School Health 89 (7): 527–35. https://doi.org/10.1111/josh.12775.
Sungwon, Kim, and Connaughton Daniel P. 2021. “Youth Soccer Parents’ Attitudes and Perceptions About Concussions.” Journal of Adolescent Health 68 (1): 184–90. https://doi.org/10.1016/j.jadohealth.2020.04.029.
Vickie, Plourde, Kung Janice Y, Gates Allison, Jun Shelly, Brooks Brian L, and Sebastianski Meghan. 2020. “How Perceptions Impact Recovery from Concussion in Childhood and Adolescence: A Systematic Review.” Neuropsychology Review 30 (1): 142–63. https://doi.org/10.1007/s11065-020-09430-y.
Zynda, Aaron J, Meagan J Sabatino, Henry B Ellis, and Shane M Miller. 2020. “Continued Play Following Sport-Related Concussion in United States Youth Soccer.” International Journal of Exercise Science 13 (6): 87–100. http://www.intjexersci.com.
Boutis, K., Weerdenburg, K., Koo, E., Schneeweiss, S., & Zemek, R. (2015). The diagnosis of concussion in a pediatric emergency department. Journal of Pediatrics, 166(5), 1214–1220.e1. https://doi.org/10.1016/j.jpeds.2015.02.013
Bramley, H., McFarland, C., Lewis, M. M., Shaffer, M. L., Cilley, R., Engbrecht, B., … Dias, M. S. (2014). Short-term outcomes of sport- and recreation-related concussion in patients admitted to a pediatric trauma service. Clinical Pediatrics, 53(8), 784–790. https://doi.org/10.1177/0009922814533403
Elbin, R. J., Sufrinko, A., Schatz, P., French, J., Henry, L., Burkhart, S., … Kontos, A. P. (2016). Removal From Play After Concussion and Recovery Time. Pediatrics, 138(3), e20160910–e20160910. https://doi.org/10.1542/peds.2016-0910
Mckinlay, A., Ligteringen, V., & Than, M. (2014). A comparison of concussive symptoms reported by parents for preschool versus school-aged children. Journal of Head Trauma Rehabilitation, 29(3), 233–238. https://doi.org/10.1097/HTR.0b013e3182a2dd7f
Taubman, B., Rosen, F., McHugh, J., Grady, M. F., & Elci, O. U. (2016). The Timing of Cognitive and Physical Rest and Recovery in Concussion. Journal of Child Neurology, 31(14), 1555–1560. https://doi.org/10.1177/0883073816664835
Terwilliger, V. K., Pratson, L., Vaughan, C. G., & Gioia, G. A. (2016). Additional Post-Concussion Impact Exposure May Affect Recovery in Adolescent Athletes. Journal of Neurotrauma, 33(8), 761–765. https://doi.org/10.1089/neu.2015.4082
Initial Medical Assessment and Management
Introduction:
At the initial assessment, verbal and written information should be shared regarding the course of recovery and about when the child/adolescent can return-to-school/activity/sport and work. Patients and their parents and/or caregivers need to know that most patients recover fully from concussion even though the recovery rate is variable and unpredictable. Providing information reduces anxiety, helps set realistic expectations, promotes recovery, and prevents re-injury.
Some children/adolescents will continue to have symptoms at one month and beyond. In these situations, the healthcare professional should refer the patient to an interdisciplinary concussion team for individualized care that targets specific prolonged symptoms. Findings from the patient’s clinical history and initial assessment can identify patients who may have an elevated risk of experiencing prolonged symptoms following concussion. Identifying patients at risk for delayed recovery in the acute stage allows for early supportive care, close monitoring for prolonged or persisting symptoms, and an opportunity to consider early referral to an interdisciplinary concussion team. For those at risk of a prolonged or persistent recovery, specialized interdisciplinary concussion care is ideally initiated within the first two weeks post-injury.
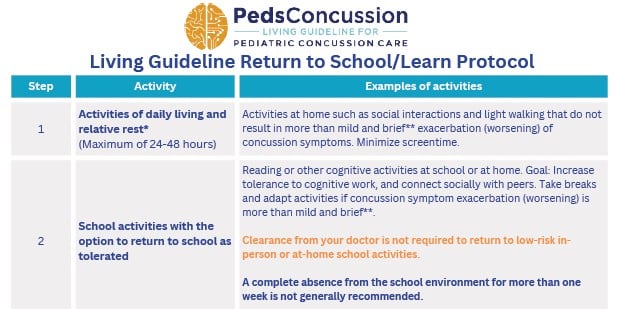
Rest beyond the first 24-48 hours after a concussion is not recommended and may cause more harm than good. Return to physical and cognitive activity should be gradual and individualized based on activity tolerance and symptom presentation (e.g., the patient is able to engage in an activity while tolerating a mild increase in symptoms). Complete absence from the school environment for more than one week is generally not recommended. The child/adolescent should gradually return to their school environment (with academic accommodations) as soon as they are able to tolerate engaging in cognitive activities, even if they are still experiencing symptoms Full-contact sport or high-risk activities where there is a risk for repeat concussion should be avoided until 1) post-concussion symptoms have subsided during both rest of physical exertion, 2) the child/adolescent has returned to full school activities without accommodations related to post-concussion symptoms, and 3) child/adolescent has medical clearance to return to full-contact sport and high-risk activities following the completion of a return-to-sport protocol.
Upon discharge from the initial assessment from the Emergency Department or Primary Care Provider (physician or nurse practitioner), families should be provided with written instructions that include red flags to return for urgent re-assessment. Families should be informed that most patients recover fully from concussion even though the recovery rate is variable; this will help set realistic expectations, promote recovery and prevent re-injury.
Recommendations
LEVEL OF EVIDENCE  A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study)
A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study) B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations)
B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations) C = Consensus, usual practice, opinion or weaker-level evidence
C = Consensus, usual practice, opinion or weaker-level evidence
2.1
Physicians or nurse practitioners should perform a comprehensive medical assessment on all children/adolescents with a suspected concussion or with acute head or spine trauma.
Include a clinical history, physical examination, and the evidence-based use of diagnostic tests or imaging as needed.
Diagnostic tools and definitions:
- 2023 American Congress of Rehabilitation Medicine Diagnostic Criteria for mTBI. Link to original paper: ACRM Criteria for Mild Traumatic Brain Injury (Figure 2 and box 1 and 2)
- Living Guideline Manage Acute and Prolonged Symptoms Algorithm
- Definition of Sport-related Concussion: 6th Consensus Statement on Concussion in Sport
2.1a
Take a comprehensive clinical history.
Level of Evidence: ![]()
Details that should be collected in the clinical history include:
- Patient demographics (e.g., age, sex, gender).
- Assess injury mechanism and symptoms at the time of injury.
- Assess symptom burden at the time of initial presentation using age-appropriate standardized symptom inventory.
- Number of symptoms.
- Severity of symptoms.
- Type of symptoms.
- Presence of loss of consciousness, post-traumatic amnesia, and red flags (seizures, neck pain, focal neurological deficits).
- Review mental health (Domain 8: Mental Health and Psychosocial Factors).
- Past medical history (e.g., previous concussions, migraine or non-specific headaches, mental health disorders, coagulopathy, other risk modifiers that may delay recovery). Note the duration until recovery from previous concussions (i.e., within 7-10 days or persisting).
- Allergies/immunizations.
- Ask whether the child/adolescent is taking any substances or medications: Prescribed or over-the-counter medications or supplements, alcohol, or recreational drugs including cannabis. These substances may mask or modify concussion symptoms.
- Ask about school, activities, work, and sports participation.
Living Guideline Tools:
- ACRM Diagnostic Criteria
- 5P Score Calculator: Validated tool identify children and youth for risk of persisting symptoms after concussion
Online resources to consider:
Standardized symptom inventory tools to consider:
- Post-Concussion Symptom Inventory (PCSI) Self-Assessment (age 5-7, 8-12, age 13-18)
- Sport Concussion Assessment Tool 6 (SCAT6 13+yrs and Child SCAT6 8-12yrs)
- Sport Concussion Office Assessment Tool (SCOAT6 13+ yrs and Child SCOAT6 8-12 yrs)
- Acute Concussion Evaluation (ACE)
2.1b
Perform a comprehensive physical examination that includes:
- Vital signs (resting heart rate and blood pressure).
- Level of consciousness (Glasgow Coma Scale).
- Mental status.
- Tool: Living Guideline Core Physical Examination: Neurological and Cervical Spine Examination
- A complete neurological examination (cranial nerve, motor, sensory, reflex, cerebellar, gait, and balance testing)
- A cervical spine examination (palpation, range of motion, provocative cervical spine tests)
- An examination of the visual and vestibular systems.
Online tools to consider:
- Living Guideline Core Physical Examination: Neurological and Cervical Spine Examination
- Sport Concussion Assessment Tool 6 (SCAT6 13+yrs and Child SCAT6 8-12yrs)
- Sport Concussion Office Assessment Tool 6 (SCOAT6 13+ yrs and Child SCOAT6 8-12 yrs)
- Heads Up to Health Care Professionals (CDC)
2.1c
Consider CT of the brain or cervical spine only in patients whom, after a medical assessment, a structural intracranial or cervical spine injury is suspected; do not conduct routine neuroimaging for the purpose of diagnosing concussion.
Most children/adolescents who sustain an acute head injury or suspected concussion do not need diagnostic imaging.
Use the following tools, as appropriate, to determine the need for CT imaging in patients with acute head trauma:
- Tool 2.2: PECARN Management Algorithm for Children after Head Trauma.
- Tool 2.3: CATCH2 Rule
- Tool 2.4: Algorithm for the Management of the Pediatric Patient ≥ 2 years with Minor Head Trauma
Although validated clinical decision-making rules are highly sensitive, these tools are meant to assist, but not replace, clinical judgment. CT scans should be used judiciously as the exposure of children/adolescents to the effects of ionizing radiation carries a small increased lifetime risk of cancer. If a structural brain injury is suspected in a patient with acute head trauma undergoing initial medical assessment in the office setting, urgent referral to an Emergency Department should be arranged.
Diagnostic imaging of the spine should be considered when symptoms are suggestive of structural cervical spine injury. Imaging should be considered in patients with severe neck pain, tenderness or clinical evidence of radiculopathy or myelopathy. The choice of imaging modality (plain radiographs, CT or MRI of the cervical spine) should be guided by the suspected pathology.
Patients with positive traumatic findings observed on diagnostic imaging of the brain or spine should be urgently referred to a neurosurgeon for consultation.
Level of Evidence: ![]() CT.
CT. ![]() MRI.
MRI.
2.1d
Note common modifiers that may delay recovery and use a clinical risk score to predict risk of prolonged symptoms.
Tool: Predicting Persistent Post-Concussive Problems in Pediatrics (5P): Score Calculator.
Modifiers that may delay recovery:
- Age (increased risk with increased age).
- Sex (female).
- Duration of recovery from a previous concussion.
- High pre-injury symptom burden.
- High symptom burden at initial presentation.
- Clinical evidence of vestibular or oculomotor dysfunction.
- Vestibular-Ocular Reflex (VOR) and tandem gait parameters.
- Orthostatic intolerance.
- Personal and family history of migraines.
- History of learning or behavioural difficulties.
- Personal and family history of mental health.
- Family socioeconomic status/education.
Level of Evidence: ![]()
2.1e
Refer patients at elevated risk for delayed recovery to an interdisciplinary concussion team.
Tool: Predicting Persistent Post-Concussive Problems in Pediatrics (5P): Score Calculator.
See Recommendation 2.1d: Note any modifiers that may delay recovery and use a clinical risk score to predict risk of prolonged symptoms.
Level of Evidence: ![]()
2.1f
Specialized interdisciplinary concussion care is ideally initiated for patients at elevated risk for a delayed recovery within the first two weeks post-injury. Level of Evidence: ![]()
See Recommendation 2.1f and Recommendation 2.1d
Tool: Predicting Persistent Post-Concussive Problems in Pediatrics (5P): Score Calculator.
2.2
Provide verbal information and written (electronic) handouts regarding the course of recovery and when the child/adolescent can return to school/activity/sport/work.
Consider the following anticipatory guidance (verbal reassurance) in order to reduce anxiety, set realistic expectations, promote recovery, and prevent re-injury:
- Tool 2.0: Living Guideline Return to Activity Sports and School Protocol
- Most patients recover fully from concussion even though the recovery rate is variable and unpredictable.
- Current symptoms are expected and common.
- The burden and distress parents/caregivers of children/adolescents who have sustained a concussion may experience is common.
- Children typically recover in 1-4 weeks but some children/adolescents will have symptoms at one month and beyond and need to be monitored/seek additional care. Females aged 13-18 years have an increased risk of prolonged recovery.
- Recommendation 2.3 Recommend graduated return to physical and cognitive activity.
- Return to school should be step-wise as soon as the student is able and include temporary academic modifications based on the student’s symptom tolerance. See Domain 12: Return-to-School and Work for more recommendations and a list of return-to-school resources.
Level of Evidence: ![]()
Online tools to consider:
- Living Guideline Patient Information Sheet
- Link: Advice for gradually resuming intellectual, physical and sports activities English/ French (INESSS)
- Link: After a Concussion: Return to Sport Strategy (Parachute Canada) (Updated in progress)
- Link: HEADS UP Resources for Returning to School (CDC)
- Link: Return to Activity Strategy (CATT)
- Link: Return-to-School Strategy (CATT)
- Link: Return to Sport Strategy (CATT)
- Link: Return to School Strategy (Parachute) (Updated in progress)
2.3
Recommend graduated return to cognitive and physical activity to promote recovery.
While most children/adolescents fully recover, the recovery rate can be variable. Return to physical and cognitive activity should be individualized based on activity tolerance and symptom presentation.
- Tool 2.0: Living Guideline Return to Activity Sports and School Protocol (Updated Sept 2023)
2.3a
Recommend an initial 24-48 hour period of relative rest*.
Level of Evidence: A Gradual return to physical activity. B Gradual return to cognitive activity.
*Relative rest: activities of daily living including walking and other light physical and cognitive activities are permitted as tolerated. (this definition has been harmonized with and adapted from the Amsterdam International Consensus Statement on Concussion in Sport)
See Living Guideline Return to Sport/Activity and School Protocols
Updated Sept 2023
2.3b
2.3b Recommend that physical and cognitive activity be started 24-48 hours after a concussion increasing the intensity gradually as part of the initial treatment for acute concussion. Activities that pose no/low risk of sustaining a concussion should be resumed even if mild residual symptoms are present.
Start with ‘light-intensity’ aerobic exercise, progressing to ‘moderate-intensity’ aerobic exercise, and continue to increase the intensity over time as symptoms are tolerated.* Suggest taking a break from the activity if the increase in symptoms is more than mild and brief** or the symptoms cannot be tolerated.
Level of Evidence: A- Physical activity, B- Cognitive activity
Updated: Sept 2023
*Light-intensity aerobic exercise: Target heart rate of up to approximately 55% of the person’s maximum heart rate (estimated according to age- 220 beats/min minus age in years)
Moderate-intensity aerobic exercise: Target heart rate of up to approximately 70% of the person’s maximum heart rate
**More than mild and brief symptom exacerbation: An increase in current concussion symptoms of no more than 2 points on a 0-10 point scale for less than an hour compared to the resting value prior to the physical activity. Example of a 0-10 point Symptom severity scale: Visual Analog Scale (VAS)
(these definitions have been harmonized with and adapted from the Amsterdam International Consensus Statement on Concussion in Sport)
- Avoid activities associated with a risk of contact, fall, or collisions (Recommendation 2.3c).
- Living Guideline Return to Activity, Sports, and School Protocol (Updated Sept 2023)
- 0-10 point Symptom severity Visual Analog Scale (VAS)
- Emphasize that spreading activities throughout the day helps patients achieve more. Tool 2.5: “Four P’s” – Prioritize, Plan, Pace, and Position.
- Domain 12: Return-to-School and Work.
- Tool 2.6: Post-Concussion Information Sheet (includes the return to activity, sports, and school protocol). (Updated Sept 2023)
- Resources: List of other evidence-based return to activity/sports strategy resources
2.3c
Recommend that patients avoid activities associated with a risk of contact, fall, or collisions such as high-speed and/or contact activities and full-contact sport that may increase the risk of sustaining another concussion until medically cleared (see Recommendation 4.1: Consider patients for medical clearance to return to full-contact activities and sport/gameplay if clinical criteria have been met. Note: An update to Rec 4.1 was performed Sept 2023).
Level of Evidence: ![]()
- Advise/emphasize that returning to full-contact sport or high-risk activities before the child/adolescent has recovered increases the risk of delayed recovery and for sustaining another more severe concussion or more serious injury.
2.3d
Refer select patients (e.g., highly-active or competitive athletes, those who are not tolerating a graduated return to physical activity, or those who are slow to recover) following acute injury to a medically supervised interdisciplinary team with the ability to individually assess aerobic exercise tolerance and to prescribe aerobic exercise treatment. This exercise tolerance assessment can be as early as 48 hours following acute injury. Level of Evidence:![]()
2.3e
2.4
Provide education and guidance regarding strategies to promote recovery.
2.4a
Advise on the importance of sleep and discuss sleep hygiene.
Level of Evidence: ![]()
Advise that consistent sleep schedules and duration of sleep may contribute to general recovery from a concussion and alleviate symptoms such as mood, anxiety, pain, fatigue, and cognitive difficulties if these are present.
Summary of tools to consider:
- Tool 2.7: Strategies to Promote Good Sleep and Alertness
- Link: Sleep for Youth. CHEO Sleep Hygiene handout
- Link: Concussion Handbook (Holland Bloorview Kids Rehabilitation Hospital)
2.4b
Advise on maintaining social networks and interactions (as tolerated). Children/adolescents should participate (modified as needed) in rewarding social activities that avoid the risk of re-injury. Social engagement may promote recovery and reduce the risk of mental health issues.
Level of Evidence: ![]()
Updated Sept 2023
2.4c
Screentime should be minimized in the first 48 hours after injury. After the initial period of relative rest, the use of devices with screens may be gradually resumed. The use of these devices can be increased according to symptom tolerance as the child/adolescent recovers.
Level of Evidence: B
Updated Sept 2023
2.4d
Advise on avoiding alcohol and other recreational drugs after a concussion.
Level of Evidence: ![]()
Alcohol and recreational drugs may have a negative effect on concussion recovery. Avoiding alcohol or drugs prevents a child/adolescent from self-medicating and resorting to drugs to relieve symptoms. Impaired judgment after a concussion could lead to risky behaviour that causes further harm or may delay the identification of complications.
2.4e
Advise to avoid driving during the first 24-48 hours after a concussion. Advise patients to begin driving when they are feeling improved, can concentrate sufficiently to feel safe behind the wheel, and when the act of driving does not provoke significant concussion symptoms.
Level of Evidence: ![]()
Provide verbal information related to when an adolescent should return to driving during recovery from a concussion. Driving is a complex coordinated process that requires vision, balance, reaction time, judgment, cognition, and attention. Concussion may have affected some or all of these skills. Driving impairments have been shown to exist even in asymptomatic patients 48 hours after a concussion. Avoiding driving for at least 24-48 hours after a concussion may potentially prevent motor vehicle accidents and, therefore, injury to the adolescent or to others.
2.5
Over-the-counter medications such as acetaminophen and ibuprofen may be recommended to treat acute headache. Limit the use of these short-term acting medications to the first week post-injury and avoid “around-the-clock” dosing to prevent overuse or rebound headaches.
Level of Evidence: ![]()
Updated Sept 2023
2.6
At present, there is limited evidence to support the administration of intravenous medication to treat acute headaches in pediatric concussion patients in the Emergency Department setting.
Level of Evidence: ![]()
2.7
After assessment, nearly all children/adolescents with concussion may be safely discharged from clinics and Emergency Departments for observation at home.
Level of Evidence: ![]()
The decision to observe in the hospital will depend on clinical judgment. Indicators for longer in-hospital observation (or to return to emergency for re-assessment) may include:
- Worsening symptoms (headache, confusion, irritability).
- Decreased level of consciousness.
- Prolonged clinical symptoms (persistent/prolonged vomiting, severe headache, etc.).
- Bleeding disorders.
- Multi-system injuries.
- Co-morbid symptoms.
Other discharge considerations:
- Observe the child/adolescent for a period of time to verify that they do not develop “red flag” symptoms prior to discharge. Use clinical judgment.
- Verify that the child/adolescent has a normal mental status (alertness/behaviour/cognition) and their symptoms are improving prior to discharge.
- Verify that an assessment of clinical risk factors indicating the need for a CT scan was performed or a normal result was obtained if a CT scan was performed prior to discharge.
- See Recommendation 2.1c for more information on when to consider diagnostic brain or cervical spine imaging.
2.8
Recommend a medical follow-up visit in 1-2 weeks to re-assess and monitor clinical status. Recommend an immediate medical follow-up in the presence of any deterioration.
Level of Evidence: ![]()
Those with a confirmed diagnosis of concussion may be managed by a healthcare professional who within their formally designated scope of practice has the capacity to manage ongoing concussion-related symptoms.
2.9
Provide post-concussion information and a written medical assessment to the child/adolescent and the parent/caregiver prior to sending the child/adolescent home.
Level of Evidence: ![]()
Write the discharge note/written medical assessment with the following information:
- The outcome of the initial medical assessment.
- Indicate to the child/adolescent and their parents, teachers, and coaches if they have been medically cleared to participate in full-contact sports or high-risk activities.
- Living Guideline Post-Concussion Information Sheet
Verbal and written (or electronic) guidance should include:
- Living Guideline Post-Concussion Information Sheet.
- An overview of common concussion symptoms.
- Warning signs that should prompt emergency medical assessment.
- Suggestions regarding activity modifications and non-pharmacological strategies to manage symptoms.
- Information on how and when to make a gradual return-to-school and low-risk physical activities. (Living Guideline Return to Activity/Sport and School Protocol
- (Domain 12: Return-to-School and Work; Recommendation 2.3: Recommend a graduated return to physical and cognitive activity).
- Information on when a medical follow-up appointment is needed (Recommendation 2.8).
Other patient information handouts to consider:
- Link: Canadian Guideline on Concussion in Sport Medical Assessment Letter (Parachute Canada).
- Link: Montreal Children’s Hospital discharge instructions.
- Link : Institut national d’excellence en sante et en services sociaux (INESSS- Québec). Advice for gradually resuming intellectual, physical and sports activities. English / French
- Link: CDC: Heads UP Discharge Instructions.
- Link: Concussion & You Handbook: Holland Bloorview Kids Rehabilitation Hospital.
- Link: Understanding and Managing Concussion in Youth: 3rd Edition Concussion Kit: Montreal Children’s Hospital.
Tools and Resources
Living Guideline Tools
- Tool 1.3 Manage Acute and Prolonged Symptoms Algorithm
- Tool 2.0: Living Guideline Return to Activity Sports and School Protocol (Updated Sept 2023)
- 2023 ACRM Diagnostic Criteria
- Tool 2.1 Physical examination
- Tool 2.2 PECARN Management Algorithm for Children after Head Trauma
- Tool 2.3 CATCH2 Rule
- Tool 2.4: Algorithm for the Management of the Pediatric Patient ≥ 2 years with Minor Head Trauma
- Tool 2.5 “Four P’s” – Prioritize, Plan, Pace, and Position
- Tool 2.6 Living Guideline Post-Concussion Information Sheet (Updated Sept 2023)
- Tool 2.7 Strategies to Promote Good Sleep and Alertness
Online Tools and Patient Handouts to Consider:
- Acute Concussion Evaluation (ACE)
- Advice for gradually resuming intellectual, physical and sports activities: Institut National d’Excellence en Santé et en Services Sociaux (INESSS- Quebec). English / French
- After a Concussion: Return to Sport Strategy (Parachute)
- Canadian Guideline on Concussion in Sport Medical Assessment Letter (Parachute)
- CATT Return to Activity Strategy
- CATT Return to Sport Strategy
- CATT Return-to-School Strategy
- CDC: Heads UP Discharge Instructions
- CDC HEADS UP Resources for Returning to School
- CDC Heads up to Health Care Professionals
- CDC mTBI Guideline Checklist
- Concussion & You Handbook: Holland Bloorview Kids Rehabilitation Hospital
- Montreal Children’s Hospital Discharge Instructions
- Parachute Return to School Strategy
- Post-Concussion Symptom Inventory (PCSI) Self-Assessment (age 5-7, 8-12, age 13-18)
- Predicting Persistent Post-Concussive Problems in Pediatrics (5P): Score Calculator
- Sport Concussion Assessment Tool 6 (SCAT6 13+yrs and Child SCAT6 8-12yrs) (Updated Sept 2023)
- Sport Concussion Office Assessment Tool (SCOAT6 13+ yrs and Child SCOAT6 8-12 yrs) (Updated Sept 2023)
- Sleep for Youth. CHEO Sleep Hygiene handout
- Understanding and Managing Concussion in Youth: 3rd Edition Concussion Kit. Montreal Children’s Hospital
References
Research papers that support the present guideline recommendations:
Aggarwal SS, Ott SD, Padhye NS, et al. Sex, race, ADHD, and prior concussions as predictors of concussion recovery in adolescents. Brain Inj. 2020 May 11;34(6):809–17.
Aggarwal, S. S., Ott, S. D., Padhye, N. S., Meininger, J. C., & Armstrong, T. S. (2019). Clinical and demographic predictors of concussion resolution in adolescents: A retrospective study. Applied Neuropsychology: Child, 8(1), 50–60. https://doi.org/10.1080/21622965.2017.1381099
Anderson V, Davis GA, Takagi M, et al. Trajectories and Predictors of Clinician-Determined Recovery after Child Concussion. J Neurotrauma. 2020 Jun 15;37(12):1392–400.
Argyropoulou MI, Alexiou GA, Xydis VG, et al. Pediatric minor head injury imaging practices: results from an ESPR survey. Neuroradiology. 2020 Feb 1;62(2):251–5.
Beauchamp, M. H., Aglipay, M., Yeates, K. O., Désiré, N., Keightley, M., Anderson, P., … Moore, J. (2018). Predictors of neuropsychological outcome after pediatric concussion. Neuropsychology, 32(4), 495–508. https://doi.org/10.1037/neu0000419
Billeck J, Peeler J. The influence of fatiguing exercise on Sport Concussion Assessment Tool (SCAT) scoring in a female pediatric population. Phys Sportsmed [Internet]. 2020 Oct 1;48(4):458–62. Available from: https://doi.org/10.1080/00913847.2020.1746979
Borland ML, Dalziel SR, Phillips N, et al. Delayed Presentations to Emergency Departments of Children With Head Injury: A PREDICT Study. Ann Emerg Med [Internet]. 2019 Jul 1;74(1):1–10. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0196064418314859
Boutis, K., Gravel, J., Freedman, S. B., Craig, W., Tang, K., DeMatteo, C. A., … Zemek, R. (2018). The Diagnosis of Concussion in Pediatric Emergency Departments: A Prospective Multicenter Study. Journal of Emergency Medicine, 54(6), 757–765. https://doi.org/10.1016/j.jemermed.2018.02.041
Boutis, K., Weerdenburg, K., Koo, E., Schneeweiss, S., & Zemek, R. (2015). The diagnosis of concussion in a pediatric emergency department. Journal of Pediatrics, 166(5), 1214–1220.e1. https://doi.org/10.1016/j.jpeds.2015.02.013
Bozan Ö, Aksel G, Kahraman HA, et al. Comparison of PECARN and CATCH clinical decision rules in children with minor blunt head trauma. Eur J Trauma Emerg Surg [Internet]. 2019 Oct 25;45(5):849–55. Available from: http://link.springer.com/10.1007/s00068-017-0865-8
Bramley, H., McFarland, C., Lewis, M. M., Shaffer, M. L., Cilley, R., Engbrecht, B., … Dias, M. S. (2014). Short-term outcomes of sport- and recreation-related concussion in patients admitted to a pediatric trauma service. Clinical Pediatrics, 53(8), 784–790. https://doi.org/10.1177/0009922814533403
Bressan S, Clarke CJ, Anderson V, et al. Use of the sport concussion assessment tools in the emergency department to predict persistent post-concussive symptoms in children. J Paediatr Child Health [Internet]. 2020 Aug 21;56(8):1249–56. Available from: https://onlinelibrary.wiley.com/doi/10.1111/jpc.14910
Brooks, T. M., Smith, M. M., Silvis, R. M., Lerer, T., Mulvey, C. H., Maitland, R., … Smith, S. R. (2017). Symptom-Guided Emergency Department Discharge Instructions for Children with Concussion. Pediatric Emergency Care, 33(8), 553–563. https://doi.org/10.1097/PEC.0000000000000797
Bunt SC, Didehbani N, Tarkenton T, et al. Sex Differences and Reporting of SCAT-5 Concussion Symptoms in Adolescent Athletes. Clin J Sport Med. 2020;Publish Ah(00).
Chan, C., Iverson, G. L., Purtzki, J., Wong, K., Kwan, V., Gagnon, I., & Silverberg, N. D. (2018). Safety of Active Rehabilitation for Persistent Symptoms After Pediatric Sport-Related Concussion: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation, 99(2), 242–249. https://doi.org/10.1016/j.apmr.2017.09.108
Chrisman SPD, Whitlock KB, Mendoza JA, et al. Corrigendum: Pilot Randomized Controlled Trial of an Exercise Program Requiring Minimal In-person Visits for Youth With Persistent Sport-Related Concussion. Front Neurol [Internet]. 2020 Feb 21;11. Available from: https://www.frontiersin.org/article/10.3389/fneur.2020.00006/full
Cohen, E., Rodean, J., Diong, C., Hall, M., Freedman, S. B., Aronson, P. L., … Neuman, M. I. (2019). Low-Value Diagnostic Imaging Use in the Pediatric Emergency Department in the United States and Canada. JAMA Pediatrics, 173(8). https://doi.org/10.1001/jamapediatrics.2019.1439
Cohrs, G., Huhndorf, M., Niemczyk, N., Volz, L. J., Bernsmeier, A., Singhal, A., … Knerlich-Lukoschus, F. (2018). MRI in mild pediatric traumatic brain injury: Diagnostic overkill or useful tool? Child’s Nervous System, 34(7), 1345–1352. https://doi.org/10.1007/s00381-018-3771-4
Corwin DJ, Arbogast KB, Swann C, et al. Reliability of the visio-vestibular examination for concussion among providers in a pediatric emergency department. Am J Emerg Med [Internet]. 2020 Sep;38(9):1847–53. Available from: https://doi.org/10.1016/j.ajem.2020.06.020
Coslick AM, Chin KE, Kalb LG, et al. Participation in Physical Activity at Time of Presentation to a Specialty Concussion Clinic Is Associated With Shorter Time to Recovery. PM R [Internet]. 2020 Dec 3;12(12):1195–204. Available from: https://onlinelibrary.wiley.com/doi/10.1002/pmrj.12443
Davis, G. A., Purcell, L., Schneider, K. J., Yeates, K. O., Gioia, G. A., Anderson, V., … Kutcher, J. S. (2017). The Child Sport Concussion Assessment Tool 5th Edition (Child SCAT5): Background and rationale. British Journal of Sports Medicine, 51(11), 859–861. https://doi.org/10.1136/bjsports-2017-097492
DeMatteo C, Bednar ED, Randall S, et al. Effectiveness of return to activity and return to school protocols for children postconcussion: a systematic review. BMJ Open Sport Exerc Med [Internet]. 2020 Feb 24;6(1):e000667. Available from: https://bmjopensem.bmj.com/lookup/doi/10.1136/bmjsem-2019-000667
Dobney, D. M., Grilli, L., Kocilowicz, H., Beaulieu, C., Straub, M., Friedman, D., & Gagnon, I. J. (2018). Is There an Optimal Time to Initiate an Active Rehabilitation Protocol for Concussion Management in Children? A Case Series. Journal of Head Trauma Rehabilitation, 33(3), E11–E17. https://doi.org/10.1097/HTR.0000000000000339
Durish, C. L., Yeates, K. O., & Brooks, B. L. (2018). Psychological Resilience as a Predictor of Persistent Post-Concussive Symptoms in Children with Single and Multiple Concussion. Journal of the International Neuropsychological Society, 24(8), 759–768. https://doi.org/10.1017/S1355617718000437
Elbin, R. J., Sufrinko, A., Schatz, P., French, J., Henry, L., Burkhart, S., … Kontos, A. P. (2016). Removal From Play After Concussion and Recovery Time. Pediatrics, 138(3), e20160910–e20160910. https://doi.org/10.1542/peds.2016-0910
Ellis, M. J., McDonald, P. J., Olson, A., Koenig, J., & Russell, K. (2019). Cervical Spine Dysfunction Following Pediatric Sports-Related Head Trauma. Journal of Head Trauma Rehabilitation, 34(2), 103–110. https://doi.org/10.1097/HTR.0000000000000411
Ellis, M., Krisko, C., Selci, E., & Russell, K. (2018). Effect of concussion history on symptom burden and recovery following pediatric sports-related concussion. Journal of Neurosurgery: Pediatrics, 21(4), 401–408. https://doi.org/10.3171/2017.9.PEDS17392
Fehr, S. D., Nelson, L. D., Scharer, K. R., Traudt, E. A., Veenstra, J. M., Tarima, S. S., … Walter, K. D. (2019). Risk Factors for Prolonged Symptoms of Mild Traumatic Brain Injury: A Pediatric Sports Concussion Clinic Cohort. Clinical Journal of Sport Medicine, 29(1), 11–17. https://doi.org/10.1097/JSM.0000000000000494
Gagnon I, Teel E, Gioia G, et al. Parent-Child Agreement on Postconcussion Symptoms in the Acute Postinjury Period. Pediatrics [Internet]. 2020 Jul;146(1):e20192317. Available from: http://pediatrics.aappublications.org/lookup/doi/10.1542/peds.2019-2317
Gauvin-Lepage, J., Friedman, D., Grilli, L., Sufrategui, M., De Matteo, C., Iverson, G. L., & Gagnon, I. (2018). Effectiveness of an Exercise-Based Active Rehabilitation Intervention for Youth Who Are Slow to Recover After Concussion. Clinical Journal of Sport Medicine, 00(00), 1. https://doi.org/10.1097/jsm.0000000000000634
Gladstone E, Narad ME, Hussain F, et al. Neurocognitive and Quality of Life Improvements Associated With Aerobic Training for Individuals With Persistent Symptoms After Mild Traumatic Brain Injury: Secondary Outcome Analysis of a Pilot Randomized Clinical Trial. Front Neurol [Internet]. 2019 Sep 18;10(September):1–9. Available from: https://www.frontiersin.org/article/10.3389/fneur.2019.01002/full
Glaviano, N. R., Benson, S., Goodkin, H. P., Broshek, D. K., & Saliba, S. (2015). Baseline SCAT2 Assessment of Healthy Youth Student-Athletes: Preliminary Evidence for the Use of the Child-SCAT3 in Children Younger Than 13 Years. Clinical Journal of Sport Medicine, 25(4), 373–379. https://doi.org/10.1097/JSM.0000000000000154
Gravel J, Ledoux AA, Tang K, et al. Early versus delayed emergency department presentation following mild Traumatic Brain Injury and the presence of symptom at 1, 4 and 12 weeks in children. Emerg Med J [Internet]. 2020 Jun;37(6):338–43. Available from: https://emj.bmj.com/lookup/doi/10.1136/emermed-2019-209054
Grool, A. M., Aglipay, M., Momoli, F., Meehan, W. P., Freedman, S. B., Yeates, K. O., … Zemek, R. (2016). Association Between Early Participation in Physical Activity Following Acute Concussion and Persistent Postconcussive Symptoms in Children and Adolescents. Jama, 316(23), 2504. https://doi.org/10.1001/jama.2016.17396
Guerriero, R. M., Kuemmerle, K., Pepin, M. J., Taylor, A. M., Wolff, R., & Meehan, W. P. (2018). The Association Between Premorbid Conditions in School-Aged Children With Prolonged Concussion Recovery. Journal of Child Neurology, 33(2), 168–173. https://doi.org/10.1177/0883073817749655
Haider MN, Johnson SL, Mannix R, et al. The Buffalo Concussion Bike Test for Concussion Assessment in Adolescents. Sport Heal A Multidiscip Approach [Internet]. 2019 Nov 5;11(6):492–7. Available from: http://journals.sagepub.com/doi/10.1177/1941738119870189
Haider MN, Worts PR, Viera KB, et al. Postexercise Slowing on the King-Devick Test and Longer Recovery From Sport-Related Concussion in Adolescents: A Validation Study. J Athl Train [Internet]. 2020 May 1;55(5):482–7. Available from: https://meridian.allenpress.com/jat/article/55/5/482/436794/Postexercise-Slowing-on-the-KingDevick-Test-and
Haider, M. N., Leddy, J. J., Wilber, C. G., Viera, K. B., Bezherano, I., Wilkins, K. J., … Willer, B. S. (2019). The predictive capacity of the buffalo concussion treadmill test after sport-related concussion in adolescents. Frontiers in Neurology, 10(APR), 1–7. https://doi.org/10.3389/fneur.2019.00395
Howell, D. R., Kriz, P., Mannix, R. C., Kirchberg, T., Master, C. L., & Meehan, W. P. (2019). Concussion Symptom Profiles Among Child, Adolescent, and Young Adult Athletes. Clinical Journal of Sport Medicine : Official Journal of the Canadian Academy of Sport Medicine, 29(5), 391–397. https://doi.org/10.1097/JSM.0000000000000629
Howell, D. R., Zemek, R., Brilliant, A. N., Mannix, R. C., Master, C. L., & Meehan, W. P. (2018). Identifying Persistent Postconcussion Symptom Risk in a Pediatric Sports Medicine Clinic. American Journal of Sports Medicine, 46(13), 3254–3261. https://doi.org/10.1177/0363546518796830
Hunt, A. W., Laupacis, D., Kawaguchi, E., Greenspoon, D., & Reed, N. (2018). Key ingredients to an active rehabilitation programme post-concussion: perspectives of youth and parents. Brain Injury, 32(12), 1534–1540. https://doi.org/10.1080/02699052.2018.1502894
Kontos AP, Jorgensen-Wagers K, Trbovich AM, et al. Association of Time Since Injury to the First Clinic Visit With Recovery Following Concussion. JAMA Neurol [Internet]. 2020 Apr 1;77(4):435. Available from: https://jamanetwork.com/journals/jamaneurology/fullarticle/2757869
Lawrence, D. W., Richards, D., Comper, P., & Hutchison, M. G. (2018). Earlier time to aerobic exercise is associated with faster recovery following acute sport concussion. PLoS ONE, 13(4), 1–12. https://doi.org/10.1371/journal.pone.0196062
Leddy, J. J., Haider, M. N., Ellis, M. J., Mannix, R., Darling, S. R., Freitas, M. S., … Willer, B. (2019). Early Subthreshold Aerobic Exercise for Sport-Related Concussion: A Randomized Clinical Trial. JAMA Pediatrics, 173(4), 319–325. https://doi.org/10.1001/jamapediatrics.2018.4397
Leddy, J. J., Haider, M. N., Hinds, A. L., Darling, S., & Willer, B. S. (2019). A Preliminary Study of the Effect of Early Aerobic Exercise Treatment for Sport-Related Concussion in Males. Clinical Journal of Sport Medicine : Official Journal of the Canadian Academy of Sport Medicine, 29(5), 353–360. https://doi.org/10.1097/JSM.0000000000000663
Leddy, J. J., Hinds, A. L., Miecznikowski, J., Darling, S., Matuszak, J., Baker, J. G., … Willer, B. (2018). Safety and prognostic utility of provocative exercise testing in acutely concussed adolescents: A randomized trial. Clinical Journal of Sport Medicine, 28(1), 13–20. https://doi.org/10.1097/JSM.0000000000000431
Ledoux, A. A., Tang, K., Yeates, K. O., Pusic, M. V., Boutis, K., Craig, W. R., … Zemek, R. L. (2019). Natural Progression of Symptom Change and Recovery from Concussion in a Pediatric Population. JAMA Pediatrics, 173(1), 1–11. https://doi.org/10.1001/jamapediatrics.2018.3820
Lindholm EB, D’Cruz R, Fajardo R, et al. Admission of Pediatric Concussion Injury Patients: Is it Necessary? J Surg Res. 2019 Dec 1;244:107–10.
Lumba-Brown, A., Yeates, K. O., Sarmiento, K., Breiding, M. J., Haegerich, T. M., Gioia, G. A., … Timmons, S. D. (2018). Diagnosis and Management of Mild Traumatic Brain Injury in Children: A Systematic Review. JAMA Pediatrics, 172(11). https://doi.org/10.1001/jamapediatrics.2018.2847
Mannix, R., Zemek, R., Yeates, K. O., Arbogast, K., Atabaki, S., Badawy, M., … Wisniewski, S. (2019). Practice patterns in pharmacological and non-pharmacological therapies for children with mild traumatic brain injury: A survey of 15 canadian and United States centers. Journal of Neurotrauma, 36(20), 2886–2894. https://doi.org/10.1089/neu.2018.6290
Master CL, Curry AE, Pfeiffer MR, et al. Characteristics of Concussion in Elementary School-Aged Children: Implications for Clinical Management. J Pediatr [Internet]. 2020;223:128–35. Available from: https://doi.org/10.1016/j.jpeds.2020.04.001
Master, C. L., Master, S. R., Wiebe, D. J., Storey, E. P., Lockyer, J. E., Podolak, O. E., & Grady, M. F. (2018). Vision and Vestibular System Dysfunction Predicts Prolonged Concussion Recovery in Children. Clinical Journal of Sport Medicine, 28(2), 139–145. https://doi.org/10.1097/JSM.0000000000000507
McCrory, P., Meeuwisse, W., Dvořák, J., Aubry, M., Bailes, J., … Vos, P.E. (2017) Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine. 51(11),838-847. https://doi.org/10.1136/bjsports-2017-097699
Mckinlay, A., Ligteringen, V., & Than, M. (2014). A comparison of concussive symptoms reported by parents for preschool versus school-aged children. Journal of Head Trauma Rehabilitation, 29(3), 233–238. https://doi.org/10.1097/HTR.0b013e3182a2dd7f
Miller, J. H., Gill, C., Kuhn, E. N., Rocque, B. G., Menendez, J. Y., O’Neill, J. A., … Johnston, J. M. (2016). Predictors of delayed recovery following pediatric sports-related concussion: a case-control study. Journal of Neurosurgery: Pediatrics, 17(4), 491–496. https://doi.org/10.3171/2015.8.PEDS14332
Olson A, Ellis MJ, Selci E, et al. Delayed Symptom Onset Following Pediatric Sport-Related Concussion. Front Neurol. 2020 Apr 3;11.
Orr, R., Bogg, T., Fyffe, A., Lam, L. T., & Browne, G. J. (2018). Graded Exercise Testing Predicts Recovery Trajectory of Concussion in Children and Adolescents. Clinical Journal of Sport Medicine, 00(00), 1. https://doi.org/10.1097/jsm.0000000000000683
Patsimas T, Howell DR, Potter MN, et al. Concussion-symptom rating correlation between pediatric patients and their parents. J Athl Train. 2020 Feb 7;55(10):1020–6.
Plourde, V., Yeates, K. O., & Brooks, B. L. (2018). Predictors of long-term psychosocial functioning and health-related quality of life in children and adolescents with prior concussions. Journal of the International Neuropsychological Society, 24(6), 540–548. https://doi.org/10.1017/S1355617718000061
Podolak OE, Chaudhary S, Haarbauer-Krupa J, et al. Characteristics of Diagnosed Concussions in Children Aged 0 to 4 Years Presenting to a Large Pediatric Healthcare Network. Pediatr Emerg Care [Internet]. 2020 Jun 16;Publish Ah. Available from: www.pec-online.com
Puffenbarger, M. S., Ahmad, F. A., Argent, M., Gu, H., Samson, C., Quayle, K. S., & Saito, J. M. (2019). Reduction of Computed Tomography Use for Pediatric Closed Head Injury Evaluation at a Nonpediatric Community Emergency Department. Academic Emergency Medicine, 26(7), 784–795. https://doi.org/10.1111/acem.13666
Root JM, McNamara B, Ledda M, et al. Pediatric Patient Compliance With Recommendations for Acute Concussion Management. Clin Pediatr (Phila). 2019 Jun 1;58(7):731–7.
Root JM, Sady MD, Gai J, et al. Effect of Cognitive and Physical Rest on Persistent Postconcussive Symptoms following a Pediatric Head Injury. J Pediatr. 2020 Dec;227:184-190.e4.
Russell, K., Selci, E., Black, B., & Ellis, M. J. (2019). Health-related quality of life following adolescent sports-related concussion or fracture: A prospective cohort study. Journal of Neurosurgery: Pediatrics, 23(4), 455–464. https://doi.org/10.3171/2018.8.PEDS18356
Schilling S, Mansour A, Sullivan L, et al. Symptom burden and profiles in concussed children with and without prolonged recovery. Int J Environ Res Public Health. 2020 Jan 1;17(1).
Stumph, J., Young, J., Singichetti, B., Yi, H., Valasek, A., Bowman, E., … Fischer, A. (2019). Effect of Exercise Recommendation on Adolescents With Concussion. Journal of Child Neurology. https://doi.org/10.1177/0883073819877790
Sutton M, Chan V, Escobar M, et al. Neck injury comorbidity in concussion-related emergency department visits: A population-based study of sex differences across the life span. J Women’s Heal. 2019 Apr 1;28(4):473–82.
Taubman, B., Rosen, F., McHugh, J., Grady, M. F., & Elci, O. U. (2016). The Timing of Cognitive and Physical Rest and Recovery in Concussion. Journal of Child Neurology, 31(14), 1555–1560. https://doi.org/10.1177/0883073816664835
Terry DP, Reddi PJ, Cook NE, et al. Acute Effects of Concussion in Youth With Pre-existing Migraines. Clin J Sport Med [Internet]. 2019 Nov 26;November. Available from: http://dx.doi.org/10.1097/JSM.0000000000000791
Terwilliger, V. K., Pratson, L., Vaughan, C. G., & Gioia, G. A. (2016). Additional Post-Concussion Impact Exposure May Affect Recovery in Adolescent Athletes. Journal of Neurotrauma, 33(8), 761–765. https://doi.org/10.1089/neu.2015.4082
Willer, B. S., Haider, M. N., Bezherano, I., Wilber, C. G., Mannix, R., Kozlowski, K., & Leddy, J. J. (2019). Comparison of Rest to Aerobic Exercise and Placebo-like Treatment of Acute Sport-Related Concussion in Male and Female Adolescents. Archives of Physical Medicine and Rehabilitation, 1–9. https://doi.org/10.1016/j.apmr.2019.07.003
Yeates, K. O., Tang, K., Barrowman, N., Freedman, S. B., Gravel, J., Gagnon, I., … Zemek, R. (2019). Derivation and Initial Validation of Clinical Phenotypes of Children Presenting with Concussion Acutely in the Emergency Department: Latent Class Analysis of a Multi-Center, Prospective Cohort, Observational Study. Journal of Neurotrauma, 36(11), 1758–1767. https://doi.org/10.1089/neu.2018.6009
Zemek, R., Barrowman, N., Freedman, S. B., Gravel, J., Gagnon, I., McGahern, C., … Moore, J. (2016). Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA – Journal of the American Medical Association, 315(10), 1014–1025. https://doi.org/10.1001/jama.2016.1203
Zou L, Li H, Jiang Z, et al. Modified decision-making rule supported by scheduled telephone follow-up reduces head computed tomography utilization in children with mild traumatic brain injury: A cohort study. Medicine (Baltimore). 2020 May 1;99(18):e20088.
Research papers not associated with a current recommendation
Bresee, N., Aglipay, M., Dubrovsky, A. S., Ledoux, A. A., Momoli, F., Gravel, J., … Zemek, R. (2018). No association between metoclopramide treatment in ED and reduced risk of post-concussion headache. American Journal of Emergency Medicine, 36(12), 2225–2231. https://doi.org/10.1016/j.ajem.2018.04.007
Corwin, D. J., Propert, K. J., Zorc, J. J., Zonfrillo, M. R., & Wiebe, D. J. (2019). Use of the vestibular and oculomotor examination for concussion in a pediatric emergency department. American Journal of Emergency Medicine, 37(7), 1219–1223. https://doi.org/10.1016/j.ajem.2018.09.008
Gravel, J., Boutis, K., Tang, K., Beauchamp, M. H., Freedman, S. B., Dubrovsky, A. S., … Zemek, R. (2019). Association between ondansetron use and symptom persistence in children with concussions: A 5P substudy. Canadian Journal of Emergency Medicine, 21(2), 204–210. https://doi.org/10.1017/cem.2018.384
Greenberg, J. K., Yan, Y., Carpenter, C. R., Lumba-Brown, A., Keller, M. S., Pineda, J. A., … Limbrick, D. D. (2018). Development of the CIDSS2 Score for Children with Mild Head Trauma without Intracranial Injury. Journal of Neurotrauma, 35(22), 2699–2707. https://doi.org/10.1089/neu.2017.5324
Howell, D. R., Potter, M. N., Kirkwood, M. W., Wilson, P. E., Provance, A. J., & Wilson, J. C. (2019). Clinical predictors of symptom resolution for children and adolescents with sport-related concussion. Journal of Neurosurgery: Pediatrics, 24(1), 54–61. https://doi.org/10.3171/2018.11.PEDS18626
Kanani, A. N., & Hartshorn, S. (2018). Resumption of physical activity within 7 days of a concussion was associated with lower rates of persistent postconcussive symptoms (PPCS). Archives of Disease in Childhood: Education and Practice Edition, 103(2), 110. https://doi.org/10.1136/archdischild-2017-313141
Lumba-Brown, A., Teramoto, M., Bloom, O. J., Brody, D., Chesnutt, J., Clugston, J. R., … Ghajar, J. (2019). Concussion Guidelines Step 2: Evidence for Subtype Classification. Neurosurgery, 0(0), 1–12. https://doi.org/10.1093/neuros/nyz332
Lyons, T. W., Miller, K. A., Miller, A. F., & Mannix, R. (2019). Racial and ethnic differences in emergency department utilization and diagnosis for sports-related head injuries. Frontiers in Neurology, 10(JUL), 1–8. https://doi.org/10.3389/fneur.2019.00690
Murdaugh, D. L., Ono, K. E., Morris, S. O., & Burns, T. G. (2018). Effects of Developmental Age on Symptom Reporting and Neurocognitive Performance in Youth After Sports-Related Concussion Compared to Control Athletes. Journal of Child Neurology, 33(7), 474–481. https://doi.org/10.1177/0883073818766815
Oyegbile, T. O., Delasobera, B. E., & Zecavati, N. (2018). Postconcussive Symptoms After Single and Repeated Concussions in 10- to 20-Year-Olds: A Cross-Sectional Study. Journal of Child Neurology, 33(6), 383–388. https://doi.org/10.1177/0883073818759436
Takagi, M., Hearps, S. J. C., Babl, F. E., Anderson, N., Bressan, S., Clarke, C., … Anderson, V. (2019). Does a computerized neuropsychological test predict prolonged recovery in concussed children presenting to the ED? Child Neuropsychology, 00(00), 1–15. https://doi.org/10.1080/09297049.2019.1639653
Date of last update: January 4, 2021
Return-to-school and Work
Introduction:
Overview:
- The return-to-school process should be coordinated by the school’s concussion management team and/or a point person in the school using the post-concussion return to school protocol and medical advice from the student’s health team (e.g., guidance counsellor, principal/vice principal, teacher, etc.).
- A key to the initial management of concussion is a gradual return to the school environment and activities after the initial period of modified activities (24-48 hours) and as soon as cognitive activities can be tolerated.
- Children/adolescents should be provided fast-acting temporary accommodations to their workload and schedule. Accommodations can be modified as symptoms resolve and/or when children/adolescents are caught up on missed workload and learning.
- Manage the gradual to school/activity/sport on a case-by-case basis.
- Post-concussion return to school and activity protocols: Living Guideline Return to School and Activities Protocols
Identifying and managing new or pre-existing school difficulties will:
- Clarify the most appropriate treatment and management options and accommodations based on the child/adolescent’s characteristics
- Promotes cognitive recovery and successful reintegration at school or work
- Support/assist return-to-school, engagement in daily activities, return to social engagement, management and treatment of symptoms
Tools to consider:
- Tool 2.0: Living Guideline Return to School and Activities Protocols (SEPT 2023 VERSION)
- Tool 1.2: Living Guideline Patient Information Sheet (SEPT 2023 VERSION)
- Tool 12.1: Concussion Implications and Interventions for the Classroom
- Tool 12.2: Template: Letter of Accommodation from the concussion care team to the school
- Tool 12.3: Template Letter of Accommodation from Physician to School
- Tool 12.4: Sample Letter/Email from School to Parents
- Link: CATT Return to School Strategy (2023 UPDATE COMING SOON)
- Link: CATT Student Return to Learn Plan (2023 UPDATE COMING SOON)
- Link: Heads Up Schools: Helping Students Recover from a Concussion: Classroom Tips for Teachers
- Link: Parachute’s Protocol for Return to Learn After a Concussion (Parachute Canada) (2023 UPDATE COMING SOON)
- Link: Post-Concussion Academic Accommodation Protocol (University of Oregon)
- Link: SCHOOLFirst: Enabling successful return to school for Canadian youth following a concussion (Holland Bloorview Kids Rehabilitation Hospital)
Recommendations
LEVEL OF EVIDENCE  A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study)
A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study) B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations)
B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations) C = Consensus, usual practice, opinion or weaker-level evidence
C = Consensus, usual practice, opinion or weaker-level evidence
12.1
This involves collaboration and communication among healthcare professionals, school-based professionals, the child/adolescent, and/or parents/caregivers.
Summary of tools to consider: These tools are suggestions for initiating a discussion to determine the best pathways for the student in learning environments.
- Tool 2.0: Living Guideline Return to School and Learn Protocol (UPDATED SEPT 2023)
- Tool 12.1: Concussion Implications and Interventions for the Classroom
- Tool 12.2: Template: Letter of Accommodation from the concussion care team to the school
- Tool 12.3: Template Letter of Accommodation from Physician to School
- Tool 12.4: Sample Letter/Email from School to Parents
- Link: CATT Return to School Strategy
- Link: CATT Student Return to Learn Plan
- Link: Heads Up Schools: Helping Students Recover from a Concussion: Classroom Tips for Teachers
- Link: Parachute’s Protocol for Return to Learn After a Concussion (Parachute Canada)
- Link: Post-Concussion Academic Accommodation Protocol (University of Oregon)
- Link: SCHOOLFirst: Enabling successful return to school for Canadian youth following a concussion (Holland Bloorview Kids Rehabilitation Hospital)
12.1a
Complete absence from the school environment for more than one week is not generally recommended. Children/adolescents should receive temporary academic accommodations (e.g, modifications to schedule, classroom environment and workload) to support a return to the school environment in some capacity as soon as possible.
Level of Evidence:![]()
- Tool 2.0: Living Guideline Return to School Protocol (UPDATED SEPT 2023)
- Tool 12.1: Concussion Implications and Interventions for the Classroom
- Tool 12.2: Template: Letter of Accommodation from the concussion care team to the school
- Tool 12.3: Template Letter of Accommodation from Physician to School
12.1b
Recommendation 2.3c: Recommend that patients avoid school activities associated with a risk of contact, fall, or collisions such as high speed and/or contact activities and full-contact sport that may increase the risk of sustaining another concussion during the recovery period. Advise/emphasize that returning to full-contact sport or high-risk activities before the child/adolescent has recovered increases the risk of delayed recovery and for sustaining another more severe concussion or more serious injury.
12.2
Assess for school difficulties using clinical judgment.
Level of Evidence: ![]()
Determine how much school the child/adolescent has missed post-concussion and how much missed workload the child/adolescent is expected to catch up on from missed school days.
Obtain school records to determine what issues may have been present prior to the concussion
School or cognitive difficulties may overlap with vision, vestibular, hearing, mental health, and social/family issues. Please assess.
- Domain 8: Mental Health
- Domain 9: Cognition
- Domain 10: Vision, Vestibular, and Oculomotor Function
12.3
Manage school difficulties.
Level of Evidence: ![]()
On re-evaluation, experienced health professionals (and school-based educational professionals where available) should manage school cognitive difficulties, provide accommodations, and reduce stressors. This should be done in collaboration with the child/adolescent, parents/caregivers, schools and/or employers to support success in the home, school, and community.
Refer to an interdisciplinary concussion team and/or a school-based educational professional (if available) if symptoms interfere with daily functioning more than 4 weeks following a concussion (Domain 9: Cognition). Refer for a formal evaluation if school difficulties may have been pre-existing.
Use tools to encourage reintegration within the school, employment, sports, social, and home environments.
Summary of tools to consider:
- Tool 2.0: Living Guideline Return to School Protocol (UPDATED SEPT 2023)
- Tool 12.1: Concussion Implications and Interventions for the Classroom
- Tool 12.2: Template: Letter of Accommodation from the Concussion Care Team to the School
- Tool 12.3: Template Letter of Accommodation from Physician to School
- Tool 12.4: Sample Letter/Email from School to Parents
- Link: SCHOOLFirst Handbook: Enabling successful return to school for Canadian youth following a concussion, page 6 (Holland Bloorview Kids Rehabilitation Hospital)
12.4
Encourage patients with school difficulties to engage in cognitive activity and low-risk physical activity as soon as tolerated. Activities that pose no/low risk of sustaining a concussion (no risk of contact, collision, or falling) should be resumed even if mild residual symptoms are present or whenever acute symptoms improve sufficiently to permit activity.
Level of Evidence: A Gradual return to physical activity. B Gradual return to cognitive activity.
See Recommendation 2.3.
12.5
Return-to-school and return-to-sport strategies can be performed simultaneously. Recommend that the child/adolescent return-to-school full-time at a full academic load, including writing exams without accommodations related to their concussion/post-concussion symptoms, before returning to full-contact sport or high-risk activities.
Level of Evidence: ![]()
See Domain 4: Medical clearance for full-contact sport or high-risk activity.
12.6
Prioritize return-to-school before return to work.
Level of Evidence: A Starting return to activity earlier.
For teens who work, please consult the “Guidelines for Concussion/ Mild Traumatic Brain Injury and Persistent Symptoms 3rd Edition For Adults (18+ years of age)” for recommendations on how to work with the adolescent’s employer regarding non-academic accommodations so that the adolescent can gradually return to work while promoting recovery.
Tools and Resources
Living Guideline Tools:
- Tool 12.1: Concussion Implications and Interventions for the Classroom
- Tool 12.2: Template: Letter of Accommodation from the Concussion Care Team to the School
- Tool 12.3: Template Letter of Accommodation from Physician to School
- Tool 12.4: Sample Letter/Email from School to Parents
Online Tools to Consider:
- CATT Return to School Strategy
- CATT Student Return to Learn Plan
- CATT Concussion Resources for School Professionals
- Heads Up Schools: Helping Students Recover from a Concussion: Classroom Tips for Teachers (CDC)
- Parachute’s Protocol for Return to Learn After a Concussion
- Post-Concussion Academic Accommodation Protocol (University of Oregon)
- SCHOOLFirst Handbook: Enabling successful return to school for Canadian youth following a concussion (Holland Bloorview Kids Rehabilitation Hospital)
References
To view and download the full citation list please use the interactive EPPImapper tool: https://pedsconcussion.com/evidence-map/
Updated list of citations included in the guideline (Sept 2023)
| Short title | Title | Year |
| Gomez (2023) | Stakeholder perspectives on navigating the pediatric concussion experience: Exploring the needs for improved communication across the care continuum | 2023 |
| Jo (2023) | Return-to-learn after sport-related concussion: does school level matter? | 2023 |
| Schmitz (2023) | Double Vision and Light Sensitivity Symptoms are Associated With Return-to-School Timing After Pediatric Concussion | 2023 |
| Shepherd (2023) | Unravelling the web: Experiences of adolescents returning to school following a concussion | 2023 |
| Vaughan (2023) | Association Between Early Return to School Following Acute Concussion and Symptom Burden at 2 Weeks Postinjury | 2023 |
| Berz (2022) | An intervention to improve knowledge and increase comfort of concussion management among school medical staff | 2022 |
| DeMatteo (2022) | School performance in youth after a concussion | 2022 |
| Kamba (2022) | Psychoeducational Interventions and Postconcussive Recovery in Children and Adolescents: A Rapid Systematic Review | 2022 |
| McAvoy (2022) | Return to Learn ECHO: Telementoring for School Personnel to Help Children Return to School and Learning After Mild Traumatic Brain Injury | 2022 |
| Mylabathula (2022) | Development of a concussion public policy on prevention, management and education for schools using expert consensus | 2022 |
| O’Brien (2022) | The School-Based Speech-Language Pathologist and Students With Concussion: An Examination of Evolving Knowledge and Confidence | 2022 |
| Takagi-Stewart (2022) | Physician recommended school accommodations and student outcomes following a mild traumatic brain injury among youth with persistent post-concussive symptoms | 2022 |
| Tang (2022) | Use of acute cognitive symptom cluster to predict return-to-learn duration following a sport-related concussion | 2022 |
| Jones (2021) | Parent and Teacher-Reported Child Outcomes Seven Years After Mild Traumatic Brain Injury: A Nested Case Control Study | 2021 |
| Keenan (2021) | Trajectories of Children’s Executive Function After Traumatic Brain Injury | 2021 |
| Yang (2021) | Association of Self-Paced Physical and Cognitive Activities Across the First Week Postconcussion With Symptom Resolution in Youth | 2021 |
| Conrick (2020) | Community-Engaged Approach to the Development and Implementation of a Student-Centered Return to Learn Care Plan After Concussion | 2020 |
| Dematteo (2020) | Effectiveness of return to activity and return to school protocols for children postconcussion: A systematic review | 2020 |
| DePadilla (2020) | Characteristics of Schools with Youth Sports Concussion-Related Educational Policies and Practices | 2020 |
| Holmes (2020) | Return to Learn: Academic Effects of Concussion in High School and College Student-Athletes | 2020 |
| Master (2020) | Characteristics of Concussion in Elementary School-Aged Children: Implications for Clinical Management | 2020 |
| Saleem (2020) | Sleep Symptoms Predict School Attendance After Pediatric Concussion | 2020 |
| Tsushima (2020) | Effects of a Single Concussion During the School Year on the Academic Performance and Neuropsychological Functioning of High School Athletes | 2020 |
| van Ierssel (2020) | Symptom Burden, School Function, and Physical Activity One Year Following Pediatric Concussion | 2020 |
| DeMatteo (2019) | Evaluating Adherence to Return to School and Activity Protocols in Children After Concussion | 2019 |
| DeMatteo (2019) | What Comes First: Return to School or Return to Activity for Youth After Concussion? Maybe We Don’t Have to Choose | 2019 |
| Gornall (2019) | Behavioral and Emotional Difficulties after Pediatric Concussion | 2019 |
| Lowry (2019) | Concussion and Academic Impairment Among U.S. High School Students | 2019 |
| Purcell (2019) | What factors must be considered in ‘return to school’ following concussion and what strategies or accommodations should be followed? A systematic review | 2019 |
| Russell (2019) | Academic outcomes following adolescent sport-related concussion or fracture injury: A prospective cohort study | 2019 |
| Sarmiento (2019) | From the CDC: A qualitative study of middle and high school professionals’ experiences and views on concussion: Identifying opportunities to support the return to school process | 2019 |
| Shendell (2019) | Developing and Piloting a School-Based Online Adolescent Student-Athlete Concussion Surveillance System | 2019 |
| Weber (2019) | School Nurses’ Management and Collaborative Practices for Student-Athletes Following Sport-Related Concussion | 2019 |
| Donnell (2018) | Concussion attitudes, behaviors, and education among youth ages 12–17: Results from the 2014 YouthStyles survey | 2018 |
| Green (2018) | Changes in working memory performance in youth following concussion | 2018 |
| Abbassi (2017) | Recovery progression and symptom resolution in sport-related mild traumatic brain injury | 2017 |
| Babcock (2017) | Adolescents with Mild Traumatic Brain Injury Get SMART: An Analysis of a Novel Web-Based Intervention | 2017 |
| Bellerose (2017) | Long-term brain-injury-specific effects following preschool mild TBI: A study of theory of mind. | 2017 |
| Rozbacher (2017) | The Effect of Concussion or Mild Traumatic Brain Injury on School Grades, National Examination Scores, and School Attendance: A Systematic Review | 2017 |
| Sufrinko (2017) | The Effectiveness of Prescribed Rest Depends on Initial Presentation After Concussion | 2017 |
| Swanson (2017) | Academic Difficulty and Vision Symptoms in Children with Concussion | 2017 |
| Ransom (2016) | Applying an Evidence-Based Assessment Model to Identify Students at Risk for Perceived Academic Problems following Concussion | 2016 |
| Russell (2016) | Academic Outcomes in High-School Students after a Concussion: A Retrospective Population-Based Analysis | 2016 |
| Wasserman (2016) | Academic Dysfunction After a Concussion Among US High School and College Students | 2016 |
| Baker (2015) | Factors Associated with Problems for Adolescents Returning to the Classroom after Sport-Related Concussion | 2015 |
| Iverson (2015) | Factors associated with concussion-like symptom reporting in high school athletes | 2015 |
| MacDonald (2015) | Reliability of a Computerized Neurocognitive Test in Baseline Concussion Testing of High School Athletes | 2015 |
| Moser (2015) | Examining prescribed rest as treatment for adolescents who are slow to recover from concussion | 2015 |
| Ransom (2015) | Academic Effects of Concussion in Children and Adolescents | 2015 |
| Ryan (2015) | Predictors of longitudinal outcome and recovery of pragmatic language and its relation to externalizing behaviour after pediatric traumatic brain injury | 2015 |
| Thomas (2015) | Benefits of Strict Rest After Acute Concussion: A Randomized Controlled Trial | 2015 |
| Van Beek (2015) | Mathematical Difficulties and White Matter Abnormalities in Subacute Pediatric Mild Traumatic Brain Injury | 2015 |
| Van Beek (2015) | Longitudinal changes in mathematical abilities and white matter following paediatric mild traumatic brain injury | 2015 |
| Brown (2014) | Effect of Cognitive Activity Level on Duration of Post-Concussion Symptoms | 2014 |
| Corwin (2014) | Characteristics of Prolonged Concussion Recovery in a Pediatric Subspecialty Referral Population | 2014 |
| Crowe (2014) | Verbal Ability and Language Outcome Following Traumatic Brain Injury in Early Childhood | 2014 |
| Darling (2014) | Evaluation of the Zurich Guidelines and Exercise Testing for Return to Play in Adolescents Following Concussion | 2014 |
| Gabbe (2014) | The association between hospitalisation for childhood head injury and academic performance: evidence from a population e-cohort study | 2014 |
| Gibson (2013) | The effect of recommending cognitive rest on recovery from sport-related concussion | 2013 |
| HOWELL (2013) | Effects of Concussion on Attention and Executive Function in Adolescents | 2013 |
Early Childhood Concussion Care
Introduction:
- Developmental considerations: Early childhood developmental stages present unique characteristics that should be considered when addressing concussion detection, assessment, monitoring of post-concussive symptoms, and recommendations for recovery.
- Language and environmental considerations: Early childhood is characterized by emerging and limited cognitive and language abilities, as well as different daily activities and environments.
- Sleep: Infants, toddlers, and preschoolers show vastly different sleep patterns compared to older individuals, including more unconsolidated sleep that includes daytime naps. Symptoms: Young children display different patterns of post-concussive symptoms than older children and adults, including unique symptoms such as elevated comfort seeking behaviors, irritability/tantrums, and regressions, that are best evaluated using observational or behavioural-anchored approaches.
- Diagnostic uncertainty: Diagnostic uncertainty tends to be more frequent in this population, leading to an increased risk of unspecified diagnosis and less precise recommendations.
- Role of parents and caregivers: Young children are entirely dependent on their parents/caregivers and other significant adults. Parental/caregiver stress can be a challenge after early childhood concussion, probably in part because parents/caregivers may struggle to identify post-concussive symptoms and concussion sequalae. It is known that parental/caregiver emotional state and parenting/caregiving behaviours influence a child’s recovery. It may be important to provide education on concussion sequela and provide guidance to parents/caregivers. Early identification and treatment of parental/caregiver stress is an important consideration.
Link: Beauchamp et al. Early Childhood Concussion, Pediatrics 2024
Recommendations
A
Concussion recognition and directing to care considerations in younger children.
As with older children, the role of caregivers, teachers, educators, and coaches is essential in ensuring concussion recognition. Concussion in early childhood primarily happens within home, childcare, or school setting. The role of parents, caregivers, educators, and teachers is especially important in detecting a suspected concussion. Provide these key interest holders with concussion recognition tools that present age-appropriate concussion signs and symptoms.
Recommended concussion tools to share with parents, educators, teachers, coaches, and other individuals working with young children;
- COCO Early childhood detection tool (English, French)
- COCO Educational kit (English, French)
- Concussion Recognition Tool-6
Tools and Resources
References