Prevention, Sport-Related Concussion, Medical Clearance to Return to High Risk Activities and Sports
Introduction
Prevention of Sport-Related Concussion
Introduction:
Section 1: What sport-related concussion (SRC) prevention strategies reduce concussion and/or head impact risk (eg, equipment, policy/rules, training strategies)?
Prevention of sport-related concussion can be considered across a spectrum and includes primary (prevention concussions in healthy individuals), secondary (preventing concussion recurrence), and tertiary (prevention of long-term consequences). All facets of injury prevention are important but shifting towards a focus on primary prevention will have the greatest public health impact in reducing the burden of concussion and its consequences. Broadly speaking, research evaluating concussion prevention strategies has considered personal protective equipment, policy and rule changes, training strategies, and management.
- Recommendations have been harmonized with and are adapted from the Amsterdam International Consensus Statement on Concussion in Sport
Section 2: Are there unintended consequences of SRC prevention strategies?
Ideally, an injury prevention program that is developed and implemented will successfully reduce injury of a specific type or population. However, it is important to consider that the same injury prevention program may inadvertently increase the risk of injury of a different injury type or to a different or future population. Continued evaluation after an injury prevention measure has been initiated remains an important aspect of prevention to ensure there are no unintended injury consequences.
Date of last update: March 2024
Recommendations
Recommendation Level of Evidence definitions: ![]() A = A Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study)
A = A Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study)![]() B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations)
B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations)![]() C = Consensus, usual practice, opinion or weaker-level evidence
C = Consensus, usual practice, opinion or weaker-level evidence
Grading of Recommendations Assessment, Development, and Evaluation (GRADE) quality rating definitions: ![]() High quality = High quality: further research is very unlikely to change our confidence in the estimate of effect.
High quality = High quality: further research is very unlikely to change our confidence in the estimate of effect.![]() Moderate quality = further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.)
Moderate quality = further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.)![]() Low quality = further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Low quality = further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.![]() Very low quality = we are very uncertain about the estimate. (See GRADE Guidelines)
Very low quality = we are very uncertain about the estimate. (See GRADE Guidelines)
Recommendation 1.1 Mouthguard use should be supported in child and adolescent ice hockey.
- (GRADE quality rating: low; Level of evidence: B).
Recommendation 1.2 Policy disallowing bodychecking should be supported for all children and most levels of adolescent ice hockey.
- (GRADE quality rating: High quality; Level of evidence: A)
Recommendation 1.3 Strategies limiting contact practice in American football should inform related policy and recommendations for all levels.
- (GRADE quality rating: low; Level of evidence: B).
Recommendation 1.4 Neuromuscular training warm-up programs are recommended, based on research in rugby, while more research is needed for females and other team sports. The focus should be on exercise components targeting concussion prevention.
- (GRADE quality rating: moderate; Level of evidence: B).
Recommendation 1.5 Policy mandating optimal concussion management strategies to reduce recurrent concussion rates is recommended.
- (GRADE quality rating: very low; Level of evidence: B).
Recommendation 2.1: Prior body checking experience in ice hockey games was not associated with lower overall concussion rates when adolescent players played in leagues permitting body checking, suggesting no overall unintended consequences of policy disallowing body checking to refuse policy recommendation above.
- GRADE quality rating: moderate; Level of evidence: B
Recommendation 2.2: Future research should consider evaluation of unintended consequences of concussion prevention strategies across all contexts.
(Recommendations are adapted from the Amsterdam International Consensus Statement on Concussion in Sport)
Tools and Resources
References
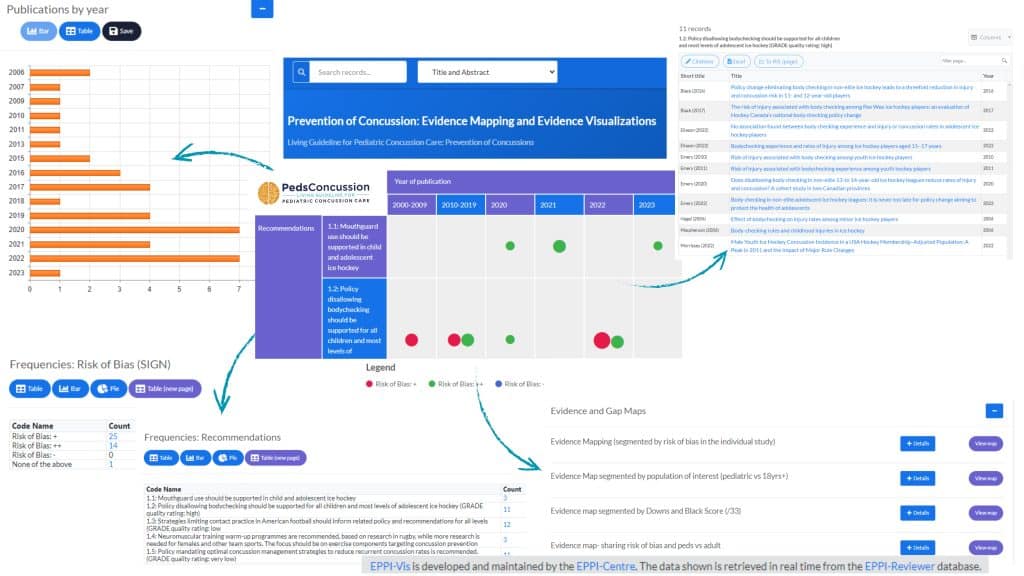
Prevention of Concussion: Living Guideline Evidence Map
Click here to access the Living Guideline Prevention of Pediatric Concussion Evidence Map (powered by EPPIreviewer and EPPIvisualizer)- View and read the evidence supporting the recommendations related to prevention of concussion (organized by recommendations, level of evidence, GRADE, bias, and publication date)
- Download RIS files, lists of all systematic reviews including, and evidence in emerging fields
Sport Concussion Considerations (baseline testing, retirement from sport, prescribed aerobic exercise)
Introduction:
Parachute Statement on Baseline Testing (Parachute Canada).
Recommendations
LEVEL OF EVIDENCE  A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study)
A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study) B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations)
B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations) C = Consensus, usual practice, opinion or weaker-level evidence
C = Consensus, usual practice, opinion or weaker-level evidence
5.1
Refer a child/adolescent with multiple concussions or baseline conditions associated with concussion-like symptoms to an interdisciplinary concussion team to help with return to full-contact sports or high-risk activities or retirement decisions from full-contact sports or high-risk activities.
Level of Evidence: ![]()
Return to full-contact sport or high-risk activity decisions can be complicated for children/adolescents with more complex medical histories. The following factors should be taken into consideration in the discussion and decisions made about return-to-sport or retirement:
- Concussion history.
- Co-morbidities (e.g., learning and communication deficits, ADHD, physical disabilities, psychiatric disorders).
- Absolute contraindications for return-to-sport and high-risk activities.
- Early recurrence or greater frequency of symptoms.
- Lower injury threshold.
- Increasing recovery time.
- Potential short- and long-term sequelae.
Some patients may benefit from neuropsychological assessment to determine resolution of cognitive problems. If a post-injury cognitive or neuropsychological assessment is deemed clinically necessary, it is recommended that this assessment be interpreted by a pediatric neuropsychologist.
5.2
Baseline testing on children/adolescents using concussion assessment tools or tests (or any combination of tests/tools) is not recommended or required for concussion diagnosis or management following an injury.
Level of Evidence: ![]()
See the Parachute Statement on Baseline Testing for more information (Parachute Canada).
“Baseline testing refers to the practice of having an athlete complete certain concussion assessment tools/tests prior to sports participation to provide baseline measurements that can be compared to post-injury values in the event of a suspected concussion. Current evidence does not support a significant added benefit of baseline testing athletes. This includes the Child SCAT5 and the SCAT5 tools, as well as neuropsychological and neurocognitive tests, both computerized or not.” (Parachute Statement on Baseline Testing)
See Recommendation 5.3: Special considerations regarding baseline testing.
5.3
Special considerations regarding baseline testing.
Level of Evidence: ![]()
Please consult the Parachute Statement on Baseline Testing for more information (Parachute Canada).
“There may be unique athlete populations and sports environments where baseline testing may be considered. These situations should be considered the exception and not the rule.”
- “Clinical neuropsychologists may consider baseline cognitive or neuropsychological testing in select youth athletes (greater than 12 years old) who have pre-existing conditions, such as a history of previous concussion, ADHD, or learning disorders, that may impact the interpretation of post-injury test results.”
- “Certain teams and sporting federations have well-established physician-supervised concussion protocols with dedicated experienced healthcare professionals working directly and continuously with youth athletes (i.e., that are present at training and competition events). In these sport environments, baseline testing may be considered as an optional assessment within the comprehensive concussion protocol as long as the medical teams caring for these athletes include experienced healthcare professionals who have competency-based training and clinical experience to allow them to administer and interpret these tests.”
(Reproduced with permission from Parachute Canada: Parachute Statement on Baseline Testing).
5.4
Recommendation 2.3d: Refer select patients (e.g., highly active or competitive athletes, those who are not tolerating a graduated return to physical activity, or those who are slow to recover) to a medically supervised interdisciplinary team with the ability to individually assess sub-symptom threshold aerobic exercise tolerance and to prescribe aerobic exercise treatment.
Level of Evidence: ![]()
Tools and Resources
Online Resource:
References
Research papers that support the present guideline recommendations:
Abeare, C. A., Messa, I., Zuccato, B. G., Merker, B., & Erdodi, L. (2018). Prevalence of invalid performance on baseline testing for sport-related concussion by age and validity indicator. JAMA Neurology, 75(6), 697–703. https://doi.org/10.1001/jamaneurol.2018.0031
Anthony, C. A., & Peterson, A. R. (2015). Utilization of a text-messaging robot to assess intraday variation in concussion symptom severity scores. Clinical Journal of Sport Medicine, 25(2), 149–152. https://doi.org/10.1097/JSM.0000000000000115
Araujo, G. C., Antonini, T. N., Monahan, K., Gelfius, C., Klamar, K., Potts, M., … Bodin, D. (2014). The relationship between suboptimal effort and post-concussion symptoms in children and adolescents with mild traumatic brain injury. Clinical Neuropsychologist, 28(5), 786–801. https://doi.org/10.1080/13854046.2014.896415
Baker, D. A., Connery, A. K., Kirk, J. W., & Kirkwood, M. W. (2014). Embedded performance validity indicators within the california verbal learning test, childrens version. Clinical Neuropsychologist, 28(1), 116–127. https://doi.org/10.1080/13854046.2013.858184
Brett, B. L., & Solomon, G. S. (2017). The influence of validity criteria on Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) test–retest reliability among high school athletes. Journal of Clinical and Experimental Neuropsychology, 39(3), 286–295. https://doi.org/10.1080/13803395.2016.1224322
Brett, B. L., Smyk, N., Solomon, G., Baughman, B. C., & Schatz, P. (2016). Long-term Stability and Reliability of Baseline Cognitive Assessments in High School Athletes Using ImPACT at 1-, 2-, and 3-year Test–Retest Intervals. Archives of Clinical Neuropsychology, (August), 904–914. https://doi.org/10.1093/arclin/acw055
Brooks, B. L., Iverson, G. L., Atkins, J. E., Zafonte, R., & Berkner, P. D. (2016). Sex Differences and Self-Reported Attention Problems During Baseline Concussion Testing. Applied Neuropsychology: Child, 5(2), 119–126. https://doi.org/10.1080/21622965.2014.1003066
Brooks, B. L., Mannix, R., Maxwell, B., Zafonte, R., Berkner, P. D., & Iverson, G. L. (2016). Multiple Past Concussions in High School Football Players. American Journal of Sports Medicine, 44(12), 3243–3251. https://doi.org/10.1177/0363546516655095
Brooks, B. L., McKay, C. D., Mrazik, M., Barlow, K. M., Meeuwisse, W. H., & Emery, C. A. (2013). Subjective, but not Objective, Lingering Effects of Multiple Past Concussions in Adolescents. Journal of Neurotrauma, 30(17), 1469–1475. https://doi.org/10.1089/neu.2012.2720
Brooks, M. A., Snedden, T. R., Mixis, B., Hetzel, S., & McGuine, T. A. (2017). Establishing baseline normative values for the child sport concussion assessment tool. JAMA Pediatrics, 171(7), 670–677. https://doi.org/10.1001/jamapediatrics.2017.0592
Chin, E. Y., Nelson, L. D., Barr, W. B., McCrory, P., & McCrea, M. A. (2016). Reliability and validity of the sport concussion assessment tool-3 (SCAT3) in high school and collegiate athletes. American Journal of Sports Medicine, 44(9), 2276–2285. https://doi.org/10.1177/0363546516648141
Collings, L. J., Cook, N. E., Porter, S., Kusch, C., Sun, J., Virji-Babul, N., … Panenka, W. J. (2017). Attention-deficit/hyperactivity disorder is associated with baseline child sport concussion assessment tool third edition scores in child hockey players. Brain Injury, 31(11), 1479–1485. https://doi.org/10.1080/02699052.2017.1377351
Cook, N. E., Huang, D. S., Silverberg, N. D., Brooks, B. L., Maxwell, B., Zafonte, R., … Iverson, G. L. (2017). Baseline cognitive test performance and concussion-like symptoms among adolescent athletes with ADHD: examining differences based on medication use. Clinical Neuropsychologist, 31(8), 1341–1352. https://doi.org/10.1080/13854046.2017.1317031
Cook, N. E., Kelshaw, P. M., Caswell, S. V., & Iverson, G. L. (2019). Children with Attention-Deficit/Hyperactivity Disorder Perform Differently on Pediatric Concussion Assessment. Journal of Pediatrics, 214, 168-174.e1. https://doi.org/10.1016/j.jpeds.2019.07.048
Covassin, T., Crutcher, B., & Wallace, J. (2013). Does a 20 minute cognitive task increase concussion symptoms in concussed athletes? Brain Injury, 27(13–14), 1589–1594. https://doi.org/10.3109/02699052.2013.823656
Custer, A., Sufrinko, A., Elbin, R. J., Covassin, T., Collins, M., & Kontos, A. (2016). High baseline postconcussion symptom scores and concussion outcomes in athletes. Journal of Athletic Training, 51(2), 136–141. https://doi.org/10.4085/1062-6050-51.2.12
Davis, G. A., Purcell, L., Schneider, K. J., Yeates, K. O., Gioia, G. A., Anderson, V., … Kutcher, J. S. (2017). The Child Sport Concussion Assessment Tool 5th Edition (Child SCAT5): Background and rationale. British Journal of Sports Medicine, 51(11), 859–861. https://doi.org/10.1136/bjsports-2017-097492
Elbin, R. J., Kontos, A. P., Kegel, N., Johnson, E., Burkhart, S., & Schatz, P. (2013). Individual and combined effects of LD and ADHD on computerized neurocognitive concussion test performance: Evidence for separate norms. Archives of Clinical Neuropsychology, 28(5), 476–484. https://doi.org/10.1093/arclin/act024
Gardner, R. M., Yengo-Kahn, A., Bonfield, C. M., & Solomon, G. S. (2017). Comparison of baseline and post-concussion ImPACT test scores in young athletes with stimulant-treated and untreated ADHD. Physician and Sportsmedicine, 45(1), 1–10. https://doi.org/10.1080/00913847.2017.1248221
Gidley Larson, J. C., Flaro, L., Peterson, R. L., Connery, A. K., Baker, D. A., & Kirkwood, M. W. (2015). The medical symptom validity test measures effort not ability in children: A comparison between mild TBI and fetal alcohol spectrum disorder samples. Archives of Clinical Neuropsychology, 30(3), 192–199. https://doi.org/10.1093/arclin/acv012
Glaviano, N. R., Benson, S., Goodkin, H. P., Broshek, D. K., & Saliba, S. (2015). Baseline SCAT2 Assessment of Healthy Youth Student-Athletes: Preliminary Evidence for the Use of the Child-SCAT3 in Children Younger Than 13 Years. Clinical Journal of Sport Medicine, 25(4), 373–379. https://doi.org/10.1097/JSM.0000000000000154
Gorman, M., Hecht, S., Samborski, A., Lunos, S., Elias, S., & Stovitz, S. D. (2017). SCAT3 assessment of non-head injured and head injured athletes competing in a large international youth soccer tournament. Applied Neuropsychology: Child, 6(4), 364–368. https://doi.org/10.1080/21622965.2016.1210011
Green, C. M., Kirk, J. W., Connery, A. K., Baker, D. A., & Kirkwood, M. W. (2014). The use of the Rey 15-Item Test and recognition trial to evaluate noncredible effort after pediatric mild traumatic brain injury. Journal of Clinical and Experimental Neuropsychology, 36(3), 261–267. https://doi.org/10.1080/13803395.2013.879096
Haider, M. N., Leddy, J. J., Pavlesen, S., Kluczynski, M., Baker, J. G., Miecznikowski, J. C., & Willer, B. S. (2018). A systematic review of criteria used to define recovery from sport-related concussion in youth athletes. British Journal of Sports Medicine, 52(18), 1179–1190. https://doi.org/10.1136/bjsports-2016-096551
Higgins, K. L., Denney, R. L., & Maerlender, A. (2017). Sandbagging on the immediate post-concussion assessment and cognitive testing (impact) in a high school athlete population. Archives of Clinical Neuropsychology, 32(3), 259–266. https://doi.org/10.1093/arclin/acw108
Iverson, G. L., Silverberg, N. D., Mannix, R., Maxwell, B. A., Atkins, J. E., Zafonte, R., & Berkner, P. D. (2015). Factors associated with concussion-like symptom reporting in high school athletes. JAMA Pediatrics, 169(12), 1132–1140. https://doi.org/10.1001/jamapediatrics.2015.2374
Kirk, J. W., Hutaff-Lee, C. F., Connery, A. K., Baker, D. A., & Kirkwood, M. W. (2014). The Relationship Between the Self-Report BASC-2 Validity Indicators and Performance Validity Test Failure After Pediatric Mild Traumatic Brain Injury. Assessment, 21(5), 562–569. https://doi.org/10.1177/1073191114520626
Kirkwood, M. W., Peterson, R. L., Connery, A. K., Baker, D. A., & Grubenhoff, J. A. (2014). Postconcussive Symptom Exaggeration After Pediatric Mild Traumatic Brain Injury. Pediatrics, 133(4), 643–650. https://doi.org/10.1542/peds.2013-3195
Kuhn, A. W., & Solomon, G. S. (2014). Supervision and computerized neurocognitive baseline test performance in high school athletes: An initial investigation. Journal of Athletic Training, 49(6), 800–805. https://doi.org/10.4085/1062-6050-49.3.66
Lichtenstein, J. D., Moser, R. S., & Schatz, P. (2014). Age and test setting affect the prevalence of invalid baseline scores on neurocognitive tests. American Journal of Sports Medicine, 42(2), 479–484. https://doi.org/10.1177/0363546513509225
Liller, K. D., Morris, B., Fillion, J., Yang, Y., & Bubu, O. M. (2017). Analysis of baseline computerized neurocognitive testing results among 5-11-year-old male and female children playing sports in recreational leagues in Florida. International Journal of Environmental Research and Public Health, 14(9). https://doi.org/10.3390/ijerph14091028
Lovell, M. R., & Solomon, G. S. (2013). Neurocognitive test performance and symptom reporting in cheerleaders with concussions. Journal of Pediatrics, 163(4), 1192–1195.e1. https://doi.org/10.1016/j.jpeds.2013.05.061
MacDonald, J., & Duerson, D. (2015). Reliability of a Computerized Neurocognitive Test in Baseline Concussion Testing of High School Athletes. Clinical Journal of Sport Medicine, 25(4), 367–372. https://doi.org/10.1097/JSM.0000000000000139
Mannix, R., Iverson, G. L., Maxwell, B., Atkins, J. E., Zafonte, R., & Berkner, P. D. (2014). Multiple prior concussions are associated with symptoms in high school athletes. Annals of Clinical and Translational Neurology, 1(6), 433–438. https://doi.org/10.1002/acn3.70
McGrath, N., Dinn, W. M., Collins, M. W., Lovell, M. R., Elbin, R. J., & Kontos, A. P. (2013). Post-exertion neurocognitive test failure among student-athletes following concussion. Brain Injury, 27(1), 103–113. https://doi.org/10.3109/02699052.2012.729282
McKay, C. D., Schneider, K. J., Brooks, B. L., Mrazik, M., & Emery, C. A. (2014). Baseline Evaluation in Youth Ice Hockey Players: Comparing Methods for Documenting Prior Concussions and Attention or Learning Disorders. Journal of Orthopaedic & Sports Physical Therapy, 44(5), 329–335. https://doi.org/10.2519/jospt.2014.5053
Moran, R. N., & Covassin, T. (2018). King-Devick test normative reference values and internal consistency in youth football and soccer athletes. Scandinavian Journal of Medicine and Science in Sports, 28(12), 2686–2690. https://doi.org/10.1111/sms.13286
Moser, R. S., Olek, L., & Schatz, P. (2019). Gender Differences in Symptom Reporting on Baseline Sport Concussion Testing Across the Youth Age Span. Archives of Clinical Neuropsychology : The Official Journal of the National Academy of Neuropsychologists, 34(1), 50–59. https://doi.org/10.1093/arclin/acy007
Moser, R. S., Schatz, P., Grosner, E., & Kollias, K. (2017). One year test–retest reliability of neurocognitive baseline scores in 10- to 12-year olds. Applied Neuropsychology: Child, 6(2), 166–171. https://doi.org/10.1080/21622965.2016.1138310
Nelson, L. D., Laroche, A. A., Pfaller, A. Y., Lerner, E. B., Hammeke, T. A., Randolph, C., … McCrea, M. A. (2015). Prospective, head-to-head study of three computerized neurocognitive assessment tools (CNTs): Reliability and validity for the assessment of sport-related concussion. Journal of the International Neuropsychological Society, 22(1), 24–37. https://doi.org/10.1017/S1355617715001101
Nelson, L. D., Loman, M. M., LaRoche, A. A., Furger, R. E., & McCrea, M. A. (2017). Baseline Performance and Psychometric Properties of the Child Sport Concussion Assessment Tool 3 (Child-SCAT3) in 5- to 13-year-old Athletes. Clinical Journal of Sport Medicine, 27(4), 381–387. https://doi.org/10.1097/JSM.0000000000000369
Nelson, L. D., Pfaller, A. Y., Rein, L. E., & McCrea, M. A. (2015). Rates and Predictors of Invalid Baseline Test Performance in High School and Collegiate Athletes for 3 Computerized Neurocognitive Tests: NAM,Axon Sports, and ImPACT. American Journal of Sports Medicine, 43(8), 2018–2026. https://doi.org/10.1177/0363546515587714
Newcomer, R. R., & Perna, F. M. (2003). Adolescent Athletes. Journal of Athletic Training, 38(2), 163–166.
Ott, S., Schatz, P., Solomon, G., & Ryan, J. J. (2014). Neurocognitive performance and symptom profiles of spanish-speaking hispanic athletes on the impact test. Archives of Clinical Neuropsychology, 29(2), 152–163. https://doi.org/10.1093/arclin/act091
Pawlukiewicz, A., Yengo-Kahn, A. M., & Solomon, G. (2017). The effect of pretest exercise on baseline computerized neurocognitive test scores. Orthopaedic Journal of Sports Medicine, 5(10), 1–6. https://doi.org/10.1177/2325967117734496
Peltonen, K., Vartiainen, M., Laitala-Leinonen, T., Koskinen, S., Luoto, T., Pertab, J., & Hokkanen, L. (2019). Adolescent athletes with learning disability display atypical maturational trajectories on concussion baseline testing: Implications based on a Finnish sample. Child Neuropsychology, 25(3), 336–351. https://doi.org/10.1080/09297049.2018.1474865
Porter, S., Smith-Forrester, J., Alhajri, N., Kusch, C., Sun, J., Barrable, B., … Virji-Babul, N. (2017). The Child Sport Concussion Assessment Tool (Child SCAT3): Normative values and correspondence between child and parent symptom scores in male child athletes. BMJ Open Sport and Exercise Medicine, 3(1), 1–6. https://doi.org/10.1136/bmjsem-2015-000029
Reesman, J., Pineda, J., Carver, J., Brice, P. J., Andrew Zabel, T., & Schatz, P. (2016). Utility of the ImPACT test with deaf adolescents. Clinical Neuropsychologist, 30(2), 318–327. https://doi.org/10.1080/13854046.2016.1142613
Reynolds, E., Fazio, V. C., Sandel, N., Schatz, P., & Henry, L. C. (2016). Cognitive Development and the Immediate Postconcussion Assessment and Cognitive Testing: A Case for Separate Norms in Preadolescents. Applied Neuropsychology: Child, 5(4), 283–293. https://doi.org/10.1080/21622965.2015.1057637
Rieger, B. P., Lewandowski, L. J., Callahan, J. M., Spenceley, L., Truckenmiller, A., Gathje, R., & Miller, L. A. (2013). A prospective study of symptoms and neurocognitive outcomes in youth with concussion vs orthopaedic injuries. Brain Injury, 27(2), 169–178. https://doi.org/10.3109/02699052.2012.729290
Sandel, N. K., Worts, P. R., Burkhart, S., & Henry, L. (2018). Comparison of baseline ImPACT performance in amateur motocross riders to football and basketball athletes. Brain Injury, 32(4), 493–497. https://doi.org/10.1080/02699052.2018.1429020
Schatz, P., & Robertshaw, S. (2014). Comparing post-concussive neurocognitive test data to normative data presents risks for under-classifying “above average” athletes. Archives of Clinical Neuropsychology, 29(7), 625–632. https://doi.org/10.1093/arclin/acu041
Schatz, P., Kelley, T., Ott, S. D., Solomon, G. S., Elbin, R. J., Higgins, K., & Moser, R. S. (2014). Utility of repeated assessment after invalid baseline neurocognitive test performance. Journal of Athletic Training, 49(5), 659–664. https://doi.org/10.4085/1062-6050-49.3.37
Snedden, T. R., Brooks, M. A., Hetzel, S., & McGuine, T. (2017). Normative Values of the Sport Concussion Assessment Tool 3 (SCAT3) in High School Athletes. Clinical Journal of Sport Medicine, 27(5), 462–467. https://doi.org/http://dx.doi.org/10.1097/jsm.0000000000000389
Snyder, A. R., & Bauer, R. M. (2014). A normative study of the sport concussion assessment tool (SCAT2) in children and adolescents. Clinical Neuropsychologist, 28(7), 1091–1103. https://doi.org/10.1080/13854046.2014.952667
Tomczyk, C. P., Mormile, M., Wittenberg, M. S., Langdon, J. L., & Hunt, T. N. (2018). An examination of adolescent athletes and nonathletes on baseline neuropsychological test scores. Journal of Athletic Training, 53(4), 404–409. https://doi.org/10.4085/1062-6050-84-17
Tsushima, W. T., Shirakawa, N., & Geling, O. (2013). Neurocognitive functioning and symptom reporting of high school athletes following a single concussion. Applied Neuropsychology: Child, 2(1), 13–16. https://doi.org/10.1080/09084282.2011.643967
Tsushima, W. T., Siu, A. M., Pearce, A. M., Zhang, G., & Oshiro, R. S. (2016). Two-year Test-Retest Reliability of ImPACT in High School Athletes. Archives of Clinical Neuropsychology, 31(1), 105–111. https://doi.org/10.1093/arclin/acv066
Tsushima, W. T., Tsushima, V. G., Oshiro, R. O., & Murata, N. M. (2017). Role of Native Language in Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) of Youth Athletes. Archives of Clinical Neuropsychology, 32(4), 450–455. https://doi.org/10.1093/arclin/acx025
Vaughan, C. G., Gerst, E. H., Sady, M. D., Newman, J. B., & Gioia, G. A. (2014). The relation between testing environment and baseline performance in child and adolescent concussion assessment. American Journal of Sports Medicine, 42(7), 1716–1723. https://doi.org/10.1177/0363546514531732
Vernau, B. T., Grady, M. F., Goodman, A., Wiebe, D. J., Basta, L., Park, Y., … Master, C. L. (2015). Oculomotor and neurocognitive assessment of youth ice hockey players: Baseline associations and observations after concussion. Developmental Neuropsychology, 40(1), 7–11. https://doi.org/10.1080/87565641.2014.971955
Womble, M. N., Reynolds, E., Schatz, P., Shah, K. M., & Kontos, A. P. (2016). Test-Retest reliability of computerized neurocognitive testing in youth ice hockey players. Archives of Clinical Neuropsychology, 31(4), 305–312. https://doi.org/10.1093/arclin/acw011
Yengo-Kahn, A. M., & Solomon, G. (2015). Are psychotropic medications associated with differences in baseline neurocognitive assessment scores for young athletes? A pilot study. Physician and Sportsmedicine, 43(3), 227–235. https://doi.org/10.1080/00913847.2015.1071638
Zalneraitis, B. H., Yengo-Kahn, A. M., Pawlukiewicz, A. J., & Solomon, G. S. (2017). Self-reported history of seizure and baseline neurocognitive test performance in student-athletes: an initial investigation. Physician and Sportsmedicine, 45(4), 470–474. https://doi.org/10.1080/00913847.2017.1372035
Date of last update: November 16, 2019
Medical Clearance for Full Contact Sport or High-Risk Activity
Introduction:
- Canadian Guideline on Concussion in Sport – 2nd Edition- Medical Clearance Letter (Parachute) (Updated March 2024)
- Concussion Recognition Tool 6. To help identify concussion in children, adolescents, and adults (Updated Sept 2023)
- Return to Sports Protocol (Updated Sept 2023)
- Amsterdam International Consensus Statement on Concussion in Sport (2023)
Recommendations
LEVEL OF EVIDENCE  A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study)
A = Consistent, good-quality, patient-oriented evidence (example: at least one large randomized control trial, meta-analysis or systematic review with homogeneity, or large, high- quality, multi-centre cohort study) B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations)
B = Inconsistent or limited-quality patient-oriented evidence (example: smaller cohort studies, case studies or control trials with limitations) C = Consensus, usual practice, opinion or weaker-level evidence
C = Consensus, usual practice, opinion or weaker-level evidence
4.1
Consider patients for medical clearance to return to full-contact activities and sport/game play if clinical criteria have been met.
The following clinical criteria should be considered or met before recommending that a child/adolescent returns to full-contact activities and sport/game play:
- ‘Return-to-Learn’: Return to pre-injury learning activities with no new academic support, including school accommodations or learning adjustments. Child/adolescent has successfully returned to all school activities including writing exams without symptoms above their previous pre-injury level or requiring accommodations related to their concussion/post-concussion symptoms, (i.e., child/adolescent may have pre-existing accommodations or new accommodations related to something other than their concussion).
- Normal neurological and cervical spine examination.
- ‘Complete symptom resolution’: Resolution of symptoms associated with the current concussion at rest with no return of symptoms during or after maximal physical and cognitive exertion (back to the pre-injury state in patients with pre-existing conditions such as baseline headaches or mental health conditions).
- Return-to-Sport: Completion of the Return to Activity/Sport protocol (2023 version) with no symptoms and no clinical findings associated with the current concussion at rest and with maximal physical exertion.
- No longer taking any drugs or substances atypical to their pre-injury functioning that could mask symptom presentation.
For children/adolescents with complex medical histories (e.g., repeated concussion, baseline concussion-like symptoms), see Recommendation 5.1 for information regarding returning to full-contact sports or high-risk activities, or retirement from full-contact sports or high-risk activities.
Definitions for ‘Complete symptom resolution’, ‘Return-to-Learn, and Return to sport have been harmonized with the Amsterdam International Consensus Statement on Concussion in Sport)
Updated Sept 2023
Level of Evidence: ![]()
For children/adolescents with complex medical histories (e.g., repeated concussion, baseline concussion-like symptoms), see Recommendation 5.1 for information regarding returning to full-contact sports or high-risk activities, or retirement from full-contact sports or high-risk activities.
4.2
Provide patients with a letter indicating medical clearance to return to all activities when medically cleared.
Level of Evidence: ![]()
Link: Canadian Guideline on Concussion in Sport Medical Clearance Letter (Parachute Canada).
4.3
Advise medically cleared patients to seek immediate medical attention if he or she develops new concussion-like symptoms or sustains a new suspected concussion.
Level of Evidence: ![]()
Tool 1.2: Concussion Recognition Tool 5. To help identify concussion in children, adolescents, and adults.
Tools and Resources
Tools to Consider:
- Canadian Guideline on Concussion in Sport Medical Clearance Letter (Parachute)
- Tool 1.2: Concussion Recognition Tool 6. To help identify concussion in children, adolescents, and adults (Updated Sept 2023)
- Tool 2.0: Return to Sports Protocol (Updated Sept 2023)
References
Research papers that support the present guideline recommendations:
Araujo, G. C., Antonini, T. N., Monahan, K., Gelfius, C., Klamar, K., Potts, M., … Bodin, D. (2014). The relationship between suboptimal effort and post-concussion symptoms in children and adolescents with mild traumatic brain injury. Clinical Neuropsychologist, 28(5), 786–801. https://doi.org/10.1080/13854046.2014.896415
Babcock, L., Kurowski, B. G., Zhang, N., Dexheimer, J. W., Dyas, J., & Wade, S. L. (2017). Adolescents with Mild Traumatic Brain Injury Get SMART: An Analysis of a Novel Web-Based Intervention. Telemedicine and E-Health, 23(7), 600–607. https://doi.org/10.1089/tmj.2016.0215
Babikian, T., McArthur, D., & Asarnow, R. F. (2013). Predictors of 1-month and 1-year neurocognitive functioning from the UCLA longitudinal mild, uncomplicated, pediatric traumatic brain injury study. Journal of the International Neuropsychological Society, 19(2), 145–154. https://doi.org/10.1017/S135561771200104X
Bonfield, C. M., Lam, S., Lin, Y., & Greene, S. (2013). The impact of attention deficit hyperactivity disorder on recovery from mild traumatic brain injury. Journal of Neurosurgery: Pediatrics, 12(2), 97–102. https://doi.org/10.3171/2013.5.PEDS12424
Brooks, B. L., Mannix, R., Maxwell, B., Zafonte, R., Berkner, P. D., & Iverson, G. L. (2016). Multiple Past Concussions in High School Football Players. American Journal of Sports Medicine, 44(12), 3243–3251. https://doi.org/10.1177/0363546516655095
Brooks, B. L., McKay, C. D., Mrazik, M., Barlow, K. M., Meeuwisse, W. H., & Emery, C. A. (2013). Subjective, but not Objective, Lingering Effects of Multiple Past Concussions in Adolescents. Journal of Neurotrauma, 30(17), 1469–1475. https://doi.org/10.1089/neu.2012.2720
Brooks, T. M., Smith, M. M., Silvis, R. M., Lerer, T., Mulvey, C. H., Maitland, R., … Smith, S. R. (2017). Symptom-Guided Emergency Department Discharge Instructions for Children with Concussion. Pediatric Emergency Care, 33(8), 553–563. https://doi.org/10.1097/PEC.0000000000000797
Collings, L. J., Cook, N. E., Porter, S., Kusch, C., Sun, J., Virji-Babul, N., … Panenka, W. J. (2017). Attention-deficit/hyperactivity disorder is associated with baseline child sport concussion assessment tool third edition scores in child hockey players. Brain Injury, 31(11), 1479–1485. https://doi.org/10.1080/02699052.2017.1377351
Cook, N. E., Huang, D. S., Silverberg, N. D., Brooks, B. L., Maxwell, B., Zafonte, R., … Iverson, G. L. (2017). Baseline cognitive test performance and concussion-like symptoms among adolescent athletes with ADHD: examining differences based on medication use. Clinical Neuropsychologist, 31(8), 1341–1352. https://doi.org/10.1080/13854046.2017.1317031
Cordingley, D., Girardin, R., Reimer, K., Ritchie, L., Leiter, J., Russell, K., & Ellis, M. J. (2016). Graded aerobic treadmill testing in pediatric sports-related concussion: safety, clinical use, and patient outcomes. Journal of Neurosurgery: Pediatrics, 18(6), 693–702. https://doi.org/10.3171/2016.5.PEDS16139
DeMatteo, C. A., Randall, S., Lin, C. Y. A., & Claridge, E. A. (2019). What comes first: Return to school or return to activity for youth after concussion? Maybe we don’t have to choose. Frontiers in Neurology, 10(JUL), 1–9. https://doi.org/10.3389/fneur.2019.00792
Donders, J., & DeWit, C. (2017). Parental ratings of daily behavior and child cognitive test performance after pediatric mild traumatic brain injury. Child Neuropsychology, 23(5), 554–570. https://doi.org/10.1080/09297049.2016.1161015
Elbin, R. J., Kontos, A. P., Kegel, N., Johnson, E., Burkhart, S., & Schatz, P. (2013). Individual and combined effects of LD and ADHD on computerized neurocognitive concussion test performance: Evidence for separate norms. Archives of Clinical Neuropsychology, 28(5), 476–484. https://doi.org/10.1093/arclin/act024
Gardner, R. M., Yengo-Kahn, A., Bonfield, C. M., & Solomon, G. S. (2017). Comparison of baseline and post-concussion ImPACT test scores in young athletes with stimulant-treated and untreated ADHD. Physician and Sportsmedicine, 45(1), 1–10. https://doi.org/10.1080/00913847.2017.1248221
Haarbauer-Krupa, J. K., Comstock, R. D., Lionbarger, M., Hirsch, S., Kavee, A., & Lowe, B. (2018). Healthcare professional involvement and RTP compliance in high school athletes with concussion. Brain Injury, 32(11), 1337–1344. https://doi.org/10.1080/02699052.2018.1482426
Haider, M. N., Leddy, J. J., Pavlesen, S., Kluczynski, M., Baker, J. G., Miecznikowski, J. C., & Willer, B. S. (2018). A systematic review of criteria used to define recovery from sport-related concussion in youth athletes. British Journal of Sports Medicine, 52(18), 1179–1190. https://doi.org/10.1136/bjsports-2016-096551
Iverson, G. L., Atkins, J. E., Zafonte, R., & Berkner, P. D. (2016). Concussion History in Adolescent Athletes with Attention-Deficit Hyperactivity Disorder. Journal of Neurotrauma, 33(23), 2077–2080. https://doi.org/10.1089/neu.2014.3424
MacDonald, J., Patel, N., Young, J., & Stuart, E. (2018). Returning Adolescents to Driving after Sports-Related Concussions: What Influences Physician Decision-Making. Journal of Pediatrics, 194, 177–181. https://doi.org/10.1016/j.jpeds.2017.10.032
Mannix, R., Iverson, G. L., Maxwell, B., Atkins, J. E., Zafonte, R., & Berkner, P. D. (2014). Multiple prior concussions are associated with symptoms in high school athletes. Annals of Clinical and Translational Neurology, 1(6), 433–438. https://doi.org/10.1002/acn3.70
Marshall CM, Chan N, Tran P, et al. The use of an intensive physical exertion test as a final return to play measure in concussed athletes: a prospective cohort. Phys Sportsmed [Internet]. 2019 Apr 3;47(2):158–66. Available from: https://www.tandfonline.com/doi/full/10.1080/00913847.2018.1542258
McCrory, P., Meeuwisse, W., Dvořák, J., Aubry, M., Bailes, J., … Vos, P.E. (2017) Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine. 51(11),838-847. https://doi.org/10.1136/bjsports-2017-097699
McKay, C. D., Schneider, K. J., Brooks, B. L., Mrazik, M., & Emery, C. A. (2014). Baseline Evaluation in Youth Ice Hockey Players: Comparing Methods for Documenting Prior Concussions and Attention or Learning Disorders. Journal of Orthopaedic & Sports Physical Therapy, 44(5), 329–335. https://doi.org/10.2519/jospt.2014.5053
Nowacki, R., van Eldik, N., Eikens, M., Roijen, R., Haga, N., Schott, D., … Wennekes, M. (2017). Evaluation of a follow-up program for mild traumatic brain injury in schoolchildren. European Journal of Paediatric Neurology, 21(2), 382–387. https://doi.org/10.1016/j.ejpn.2016.10.009
Reed, N., Taha, T., Monette, G., & Keightley, M. (2016). A Preliminary Exploration of Concussion and Strength Performance in Youth Ice Hockey Players. International Journal of Sports Medicine, 37(9), 708–713. https://doi.org/10.1055/s-0042-104199
Root, J. M., Zuckerbraun, N. S., Wang, L., Winger, D. G., Brent, D., Kontos, A., & Hickey, R. W. (2016). History of Somatization Is Associated with Prolonged Recovery from Concussion. Journal of Pediatrics, 174, 39–44.e1. https://doi.org/10.1016/j.jpeds.2016.03.020
Sady, M. D., Vaughan, C. G., & Gioia, G. A. (2014). Psychometric characteristics of the postconcussion symptom inventory in children and adolescents. Archives of Clinical Neuropsychology, 29(4), 348–363. https://doi.org/10.1093/arclin/acu014
Salinas, C. M., Dean, P., LoGalbo, A., Dougherty, M., Field, M., & Webbe, F. M. (2016). Attention-Deficit Hyperactivity Disorder Status and Baseline Neurocognitive Performance in High School Athletes. Applied Neuropsychology: Child, 5(4), 264–272. https://doi.org/10.1080/21622965.2015.1052814
Tamura K, Furutani T, Oshiro R, et al. Concussion recovery timeline of high school athletes using a stepwise return-to-play protocol: Age and sex effects. J Athl Train [Internet]. 2020 Jan 1;55(1):6–10. Available from: https://meridian.allenpress.com/jat/article/55/1/6/433840/Concussion-Recovery-Timeline-of-High-School
Date Updated: January 4, 2021